Bone Grafting or No Bone Grafting? A Common Dental Implant Dilemma
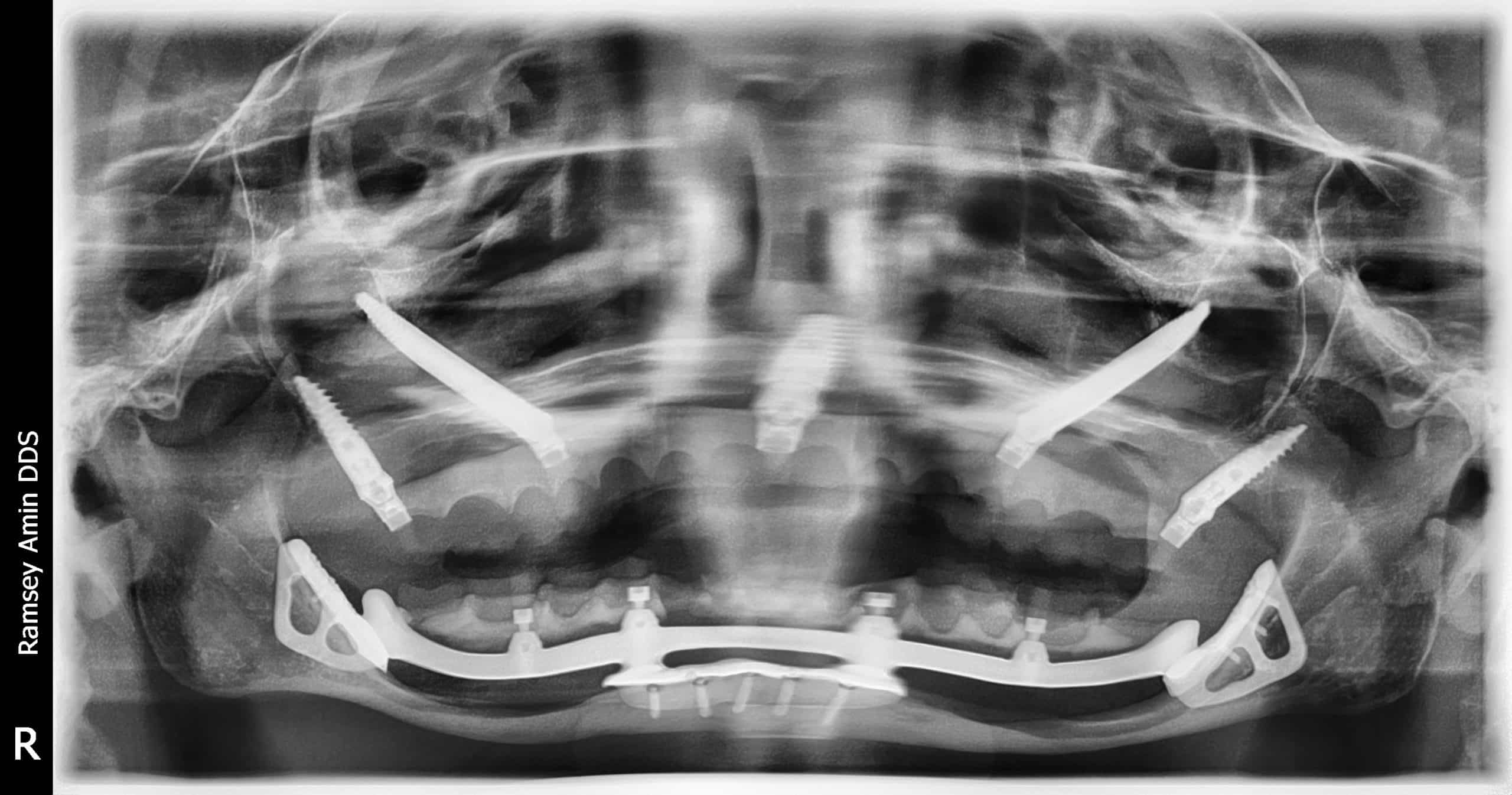
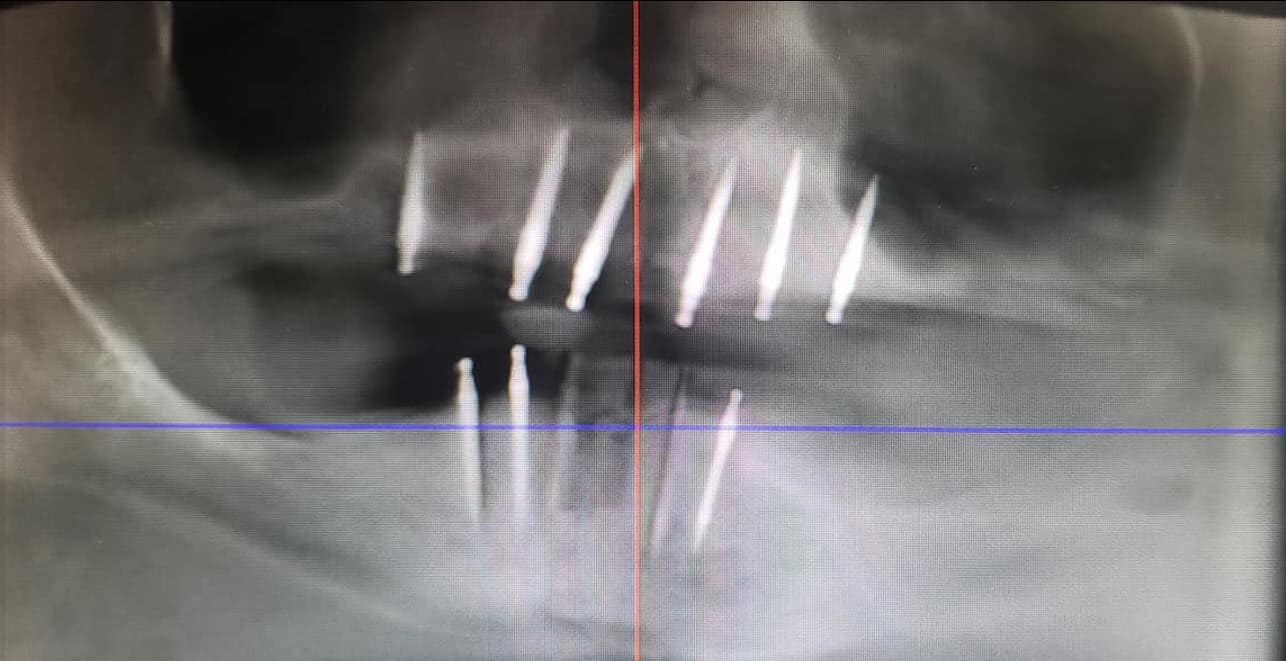
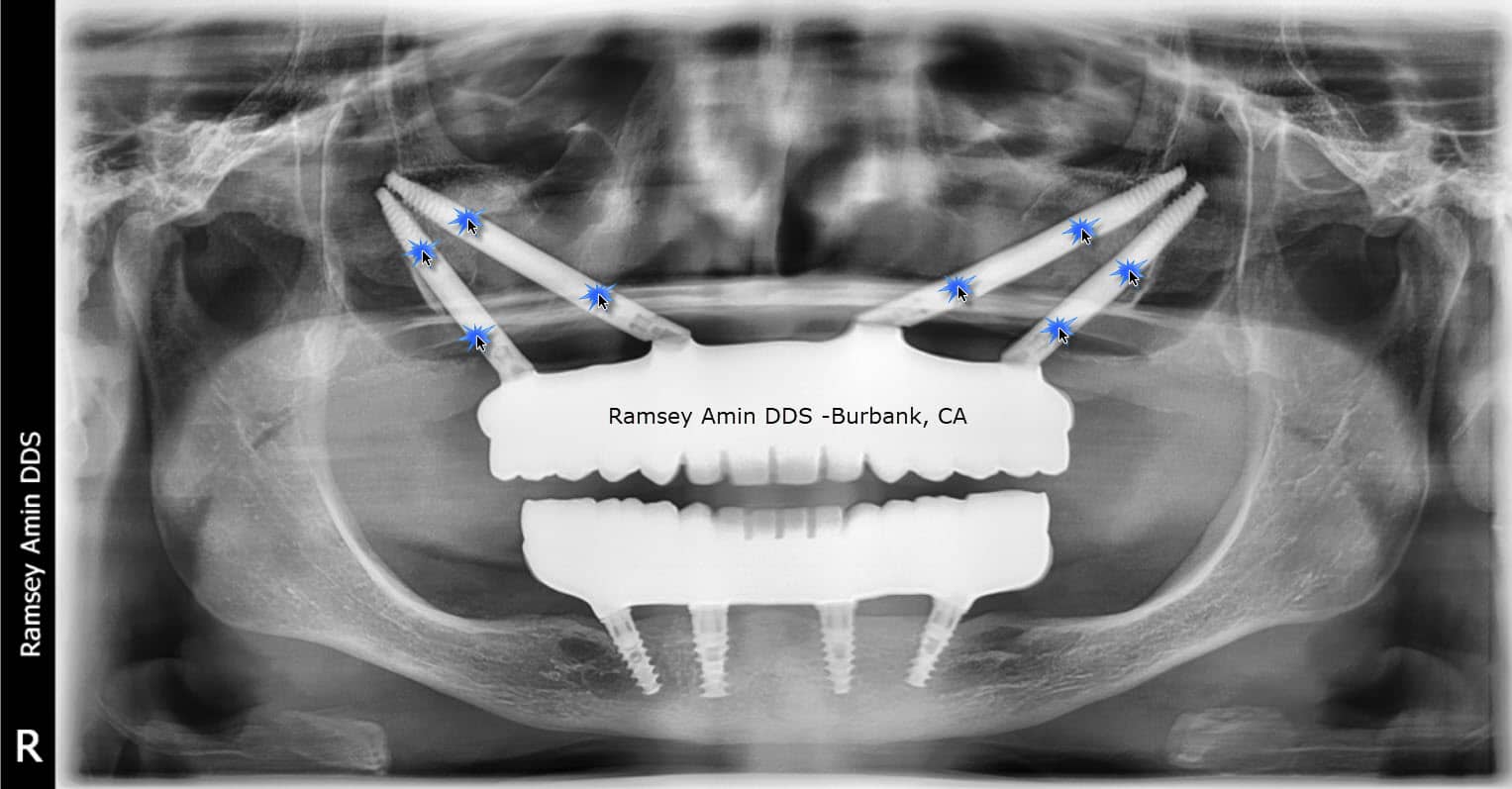
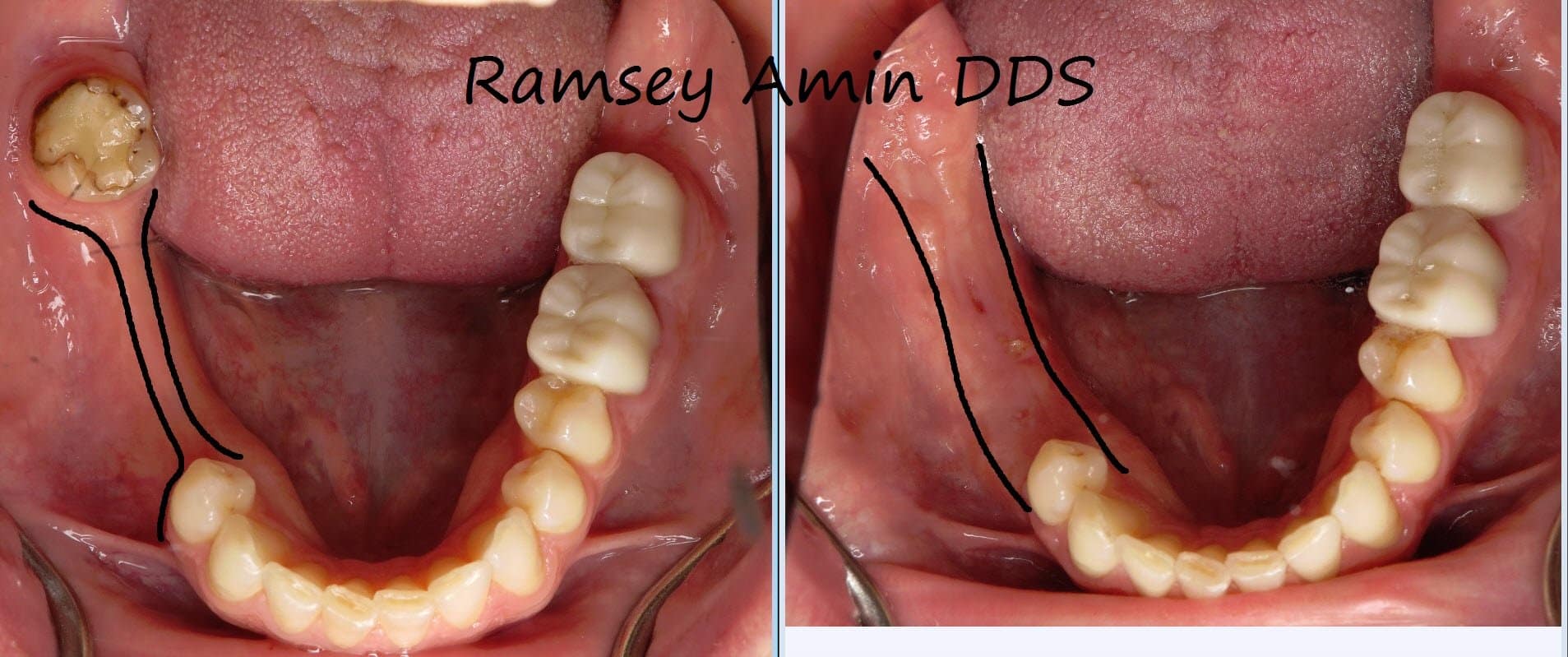
This patient has severe bone loss of the lower front teeth area. He wants implants, but was told by numerous dentists it could not be done. A huge part of my practice in Burbank, California is devoted to treating these very difficult dental implant cases where huge bone grafts may be needed. I was confident … Read more