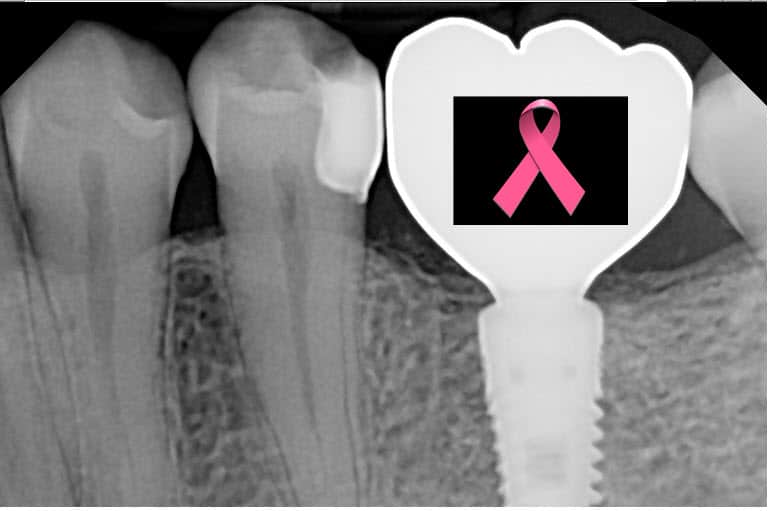
Chemotherapy and Dental Implants – Can Cancer Patients Get Dental Implants (Special Emphasis on Breast Cancer)?
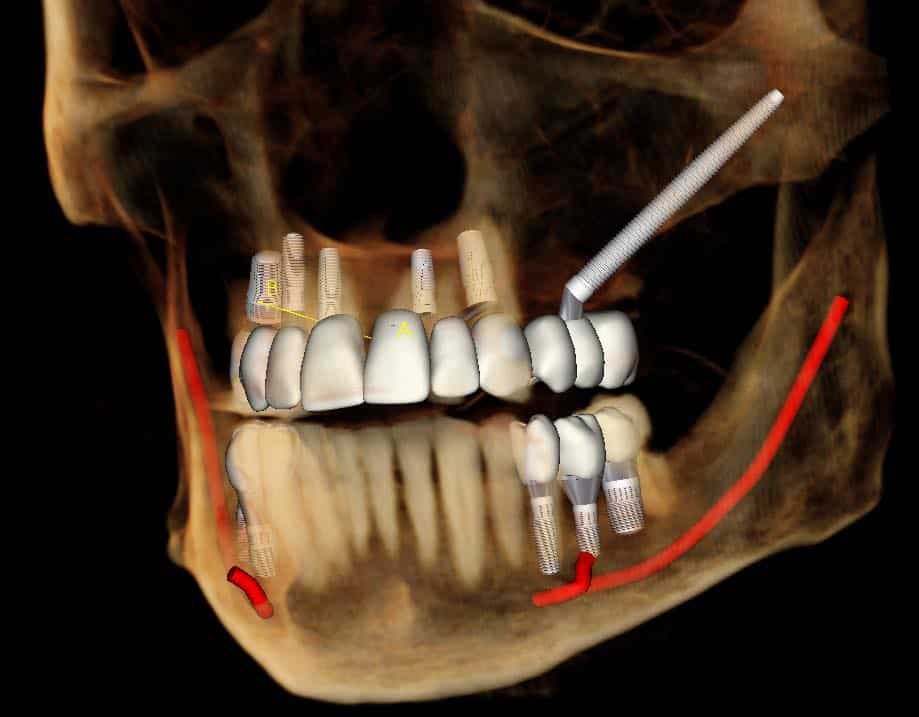
As a cancer survivor, replacing any teeth you lost before, during or after treatment can be an important part of regaining your health and quality of life. For many patients, dental implants are an excellent option – but the process requires some special considerations for cancer patients (i.e. is it possible for chemotherapy and dental … Read more