Full Arch Implant – A Difficult Case Explained (No Bone, Underbite)
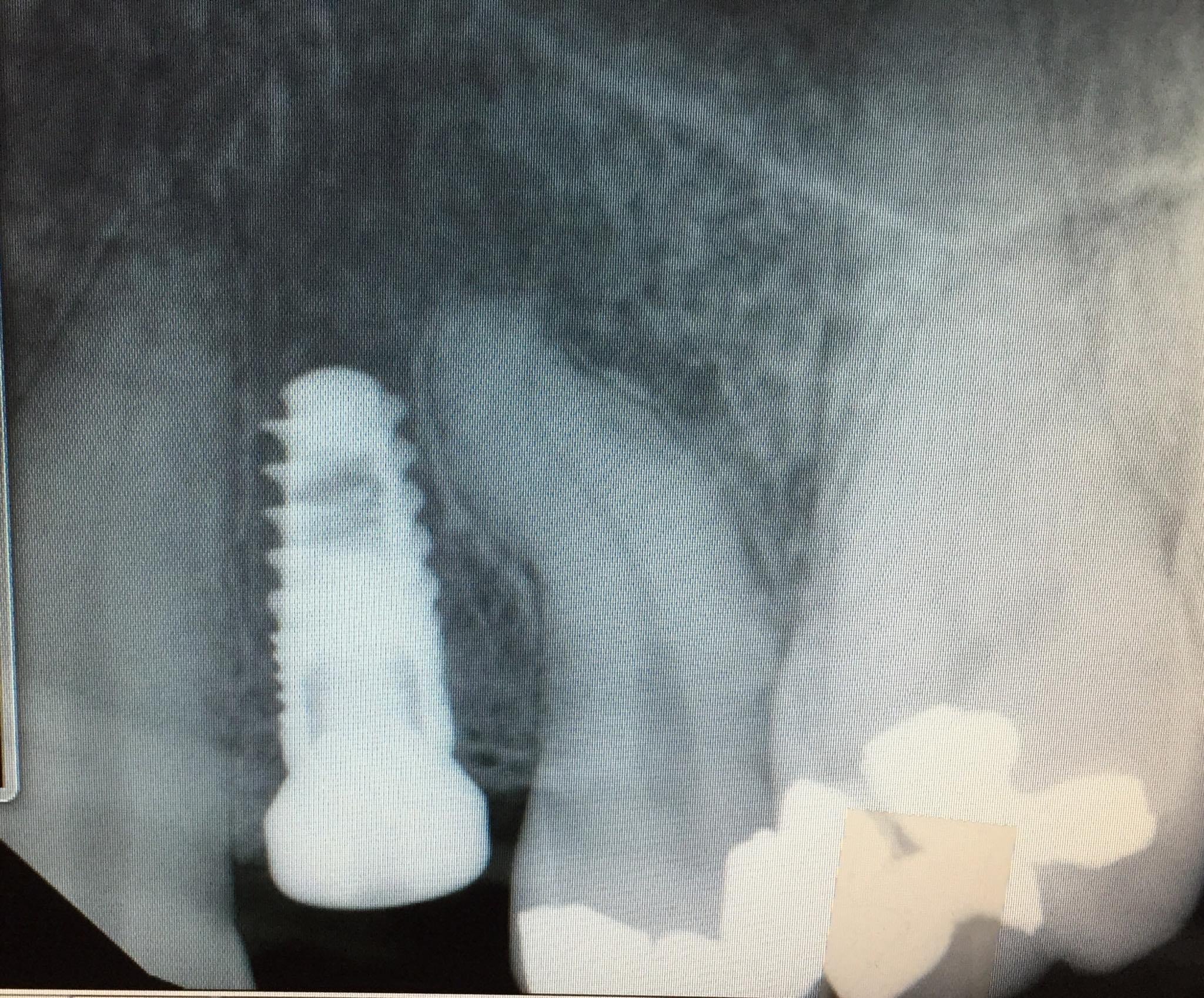
This is a difficult full arch implant case with a full upper arch reconstruction utilizing the zygomatic and pterygoid dental implants. Let me explain why this case is more difficult than average. She was told by two other offices that they could only make her a snap-on denture. My office in Burbank, California was her … Read more