(updated July 2022)
Dental implants can be problematic if you take Fosamax, Actonel or Boniva. So can you get dental implants if you have osteoporosis?
Contrary to popular opinion, having osteoporosis does not mean you cannot have dental implants, sinus lifts or bone grafts.
If you’ve taken those medications (called bisphosphonates) to treat osteoporosis, you can still get dental implants (choose an experienced implant dentist for best results!).
Need dental implants, but also take bisphosphonates?
For more than a decade, I have safely placed dental implants on patients who take or have taken these medications.
Oral bisphosphonates like Fosamax, Actonel and Boniva are commonly used for the prevention and treatment of osteoporosis. They work by preventing bone breakdown and increasing bone density (thickness).
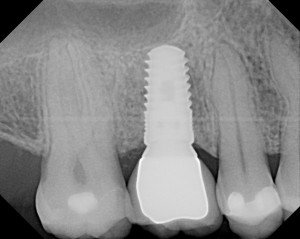
This sounds great, but when having a dental implant, bone graft or extraction, you need to have both types of cells that make bone and remove bone in order to heal normally.
Your risk involving dental implants while having osteoporosis
Having been treated previously or currently with bisphosphonate drugs you should know that there is a risk of future complications associated with dental implants, bone grafting or oral surgery treatment.
Fosamax-type drugs appear to adversely affect the ability of the jawbone to break down or remodel itself, thereby reducing or eliminating its ordinary excellent healing capacity.
The risk is a lot less if you only have osteoporosis and not too many other medical conditions that can add risk.
This risk is increased after surgery, especially from tooth extraction, implant placement or other “invasive ” procedures that might cause even mild trauma to bone.
The risk is significantly higher in patients who have received the injectable (IV) forms of these drugs (Zometa is an IV type).
Osteonecrosis may result. This is a smoldering, long-term, destructive process in the jawbone that is often very difficult or impossible to eliminate. The bone becomes exposed in the mouth and the gum doesn’t heal over it.
Fortunately this complication is fairly uncommon and happens in only about 1% of cases. I have personally seen it. It is most common in the lower jaw as opposed to the upper jaw.
The risk of osteonecrosis after having a dental implant is increased if you have been taking it longer than 3-4 years.
Fosamax , Actonel and Boniva last in your bone long after you stopped taking it. It may last in your bone for 10-50 years!
Make Sure Your Implant Dentist Knows Your Medical History
Your medical/dental history is very important to me. Let me know if you take or have taken Fosamax , Actonel and Boniva before a sinus lift, bone graft or dental implant.
I may write you a prescription to have a special blood test to check your risk before we start. I may consult with your medical doctor to modify your regimen.
It is critical to choose a very knowledgeable implant dentist when you have taken these types of medications because there are many other factors that can cause problems not listed above.
Also, be sure to check out the article I wrote and published on the The American Academy of Implant Dentistry website (you can read it here).
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow of the American Academy of Implant Dentistry
Burbank, California

Hi Dr. Amin. I’m so grateful that my research led me to you and your works prior to obtaining all-on-four/six implants. I have severe osteoporosis for which my doctor has prescribed a potent medication, Forteo (a parathyroid hormone, teriparatide). Although your articles cover the risks involved with bisphosphonate and implants, I have not been able to find anything on this particular pharmaceutical compound. Do you have or can you direct me to any current information and/or studies on it? Also, do you by any chance know of any dentists in the New Jersey area who share your expertise on the topic?
Forteo has less of an affect on the dental treatment than the classic medications. It all depends on what else you are taking and what OTHER medical conditions you have besides osteoporosis. It is not exactly black or white. It has to be case-by-case and patient by patient.
Hi. I’m planning on getting an implant in my lower jaw and was wondering when it would be recommended to start the Zometa infusions that my oncologist wants me to start? She wants me to get the infusions every 6 months for 3 years. I don’t have osteoporosis, but since I’ve been put into menopause… she wants to protect my bones. I’m worried about the implant failing, or that I wouldn’t be able to get any future major dental work. What are your thoughts?
Avoid Zometa! Why not use weaker oral medications rather than the silver bullet injectible Zometa? Seems like a shotgun approach that will make dentistry challenging!
Hi doctor I am 36 male , had 6 rcts in 12 years and one dental implant , at this age by chance I found out that I have osteoporosis in my lumber spine, and osteopina in hip joint , I am quite devastated as I am healthy looking person and always had healthy life style never smoke, or consume alcohol never had steroids or any health issues , doctor prescribed me fosamax and I am quite reluctant to do, my vit d level were severely low 7.5ng/ml, so I started working on them, while every other test is perfectly normal, should I start medicine and within two years can I do any dental work ? Chances of jaw necrosis ? Kindly advice me.
Hi doctor I am 36 male , had 6 rcts in 12 years and one dental implant , at this age by chance I found out that I have osteoporosis in my lumber spine, and osteopina in hip joint , I am quite devastated as I am healthy looking person and always had healthy life style never smoke, or consume alcohol never had steroids or any health issues , doctor prescribed me fosamax and I am quite reluctant to do, my vit d level were severely low 7.5ng/ml, so I started working on them, while every other test is perfectly normal, should I start medicine and within two years can I do any dental work ? Chances of jaw necrosis ? Kindly advice me.
Yes start the meds !
Taking care of your bones is more important than your teeth especially if you have osteopenia at such a young age and osteoporosis.
Your dental work can be managed even if you take these medications. I would just suggest you see a very skillful dentist who is knowledgeable in these bisphosphonate medications. 😊
I’ve been on Alendrolate 70mg, 1x/wk for @2.5 yrs for osteoporosis. I had an extraction for cracked tooth (upper, 4th from center), in July with oral surgeon. He did bone graft, as the plan is for an implant next month. Now, reading this, I am not sure if I should have the implant.
I had no problems with the bone graft. I think he is aware of the med, but it was not brought up.
Should I stop the med? I have 5wks before the implant. Thank you.
2.5-3 years is where we begin to see some problems mostly on the lower teeth and again the risk is pretty remote if you are only taking the oral pills rather than the injectables. If he healed well from the extraction likely all should be good but certainly this is something to discuss with your dentist and medical doctor. Sometimes a “drug holiday” is a good thing. I am hoping you are not on a steroid as well for something else.
Greetings. I took Fosamax for 7 years and stopped in 2010. I am female 64 years old. I am needing an extraction and my dentist is recommending a bridge instead of implant due to Fosamax use. I’d prefer an implant and also highly trust my dentist. What blood test are you referring to and what exactly does it show? Would you consider an implant in my case? It was oral Fosamax, not injectable. Thanks so much.
There is much more to this! Besides osteoperosis, list ALL other medications and health problems you have.
Many patients on fosamax can very safely have implants! I do them EVERY day!
Hello Doctor
60 yo male with osteoporosis, hip fracture after a fall three years ago, :-/ , many implants and crowns already. My bone density is stable since then. Dr wants me to start forteo for 2 years and follow up with IV Reclast, but I’m obviously reluctant. What do you think of this regimen considering that I’m likely to need more implants in the coming years? Thank you
Yikes. reclast is the bad one!! This will pretty much prohibit you from having implants for quite a long time depending on your dose regimen
Of course breaking a hip is more important then a tooth. You need to speak to your doctor about all of this
Not as common in males but it does happen
Obviously weight-bearing exercises along with vitamin D and calcium or some of the non-pharmaceutical ways to help.
👍🏻😁
Hello Doctor,
My mom had 5 implants placed in her lower jaw and a bone graft, but the doctor did not ask us about her medical history.
She has osteoporosis and was on actonel for 8 months the last dose she took was 1 1/2 months before the procedure.
Will it lead to any complications in her case.
🙏🙏hopefully will be ok.
That dose is not as bad as being on it 3-4 years straight.
As long as she doesn’t have other medical issues that make it worse she should be ok.
😁
I am 47 years old. I was diagnosed with osteoporosis 4 months ago when I started taking weekly Fosamax. I am considering an implant. Wondering if 4 months of Fosamax will interfere with the implant process and healing.
Not so much since it has only been 4 months …but you still
Have less bone forming cells than someone without osteoporosis.
See someone with a lot of experience
Hello Doctor
I took my first shot of prolia 5 months ago, can I have tooth implant now? and should i go to a dentist or periodontist for the implant ?
thanks
There are many dentists that do implants. There is a wide variety of experience, training and judgment. Here is an article that will help you understand how to choose a dental implant dentist.
If you are currently on Prolia I’m willing to bet you took Fosamax and/or Boniva in the past. Regardless of who you see I would suggest they are well-versed in the bisphosphonate medicines and their effect on dental implant healing. Complications could be significant especially if you’re having an implant on the lower jaw.
I have been on Risenodrate for 8 months and want to have Invisalign done. How long do I need to be off of the medicine before I can start the Invisalign?
Talk to the orthodontist, but I personally don’t think it will affect it.
I was on Alendronate for 4 months and then stopped taking it as my teeth felt loose. It has another 4 months since I stopped taking it. My teeth still feel loose and have trouble chewing. Will my loose teeth ever get strong again? Will I be able to chew food?
Please email me the reply.
Thanks.
Chance that this is related is about 1 %. You likely had periodontal gum disease before and are now just noticing it.
I was on Fosomax then Boniva for about 8 years for osteopenia diagnosed in my mid 30’s. I was taken off of it about 8 years ago. I was just diagnosed with osteopenia again ((had several stress fractures over last 6 months). My doctor prescribed me Boniva again. I had a dental implant a little over 1-1/2 years ago. As far as I know everything is healed. Should it be safe enough now to take Boniva? I really don’t want to have problems with the implant.
Great question and very well described. If the implant has integrated it would be fine to go back onto Boniva if they really feel that is going to help you with your osteoporosis. Just be careful with injectable bisphosphonates such as Zometa as they have a much higher incidence of causing bone issues in the mouth. I am assuming you have tried Forteo and other monoclonal antibody medications.
Hi, my question is I already have dental implants for my lower teeths with a complete denture. My rheumatologist doctor found that my bone density is too low, is there a chance to lost my dental implanti if I start taking prolia injections for my osteoporosis in my hip. There is a chance to have different methods (natural medication to increase the bone density).
That is a question for your Dr. about increasing her bone density but typically most females that are postmenopausal typically supplement with vitamin D, calcium and magnesium. These are potent supplements and for some people can actually cause problems. Be sure to talk to Dr. about this and of course about weightbearing exercise to build bone.
I was on Reclast for 5 years and have been off of it for 3.
I am recuperating from a dental implant lower front (5 days).
My dentist knew my history did only X-rays no blood test.
I am on antibiotics. I’m in a lot of pain but everything looks good and seems to be healing.
After reading all this information I’m terrified. Is there anything I should be watching for regarding complications.
yikes….fortunately you have been off of it for 3 years but the medicine Reclast is intravenous Zometa. This is a very powerful bisphosphonate. I suggest you see your dentist for a follow-up at the minimum every 5 days and consider being on antibiotics for at least 2 weeks. I am hoping you do not have a removable temporary on top of the implant that was placed. Do not put anything over it that could pull the gums apart and exposed the bone more than it has already. Fortunately, not everybody gets the complication. Please keep me posted and when you do post please describe your history again
I am 37 yrs old woman. I removed lower left wisdom tooth. I want to know after how much time can I restart my fosamax again. My endocronologist says that I am in menopause and wants to start fosamax for bone strength. I had been taking fosamax for 3 yrs. I stopped taking fosamax 4 months before I removed my wisdom tooth.
6 weeks
Dr. Amin,
I am a 64 year old woman recently diagnosed with osteoporosis. My doctor wants me to start Fosamax for a 5 year duration. I had 2 failed root canals (#15 due to missed canal and #30 due to a no longer used endodonic filling material that never hardened in the middle). I had them both redone a couple of years ago. The are slowly healing. Both still show periapical shadowing, more on #30. Endodontist says bone on #15 is slowly filling in, said #30 is ‘functional’. My concern is this could be a risk for ONJ because the root canals are a few years old and I worry about any possible remaining infection in the bone. (as a side note, I am about 1 year into Invisalign treatment). Any advice/comments would be greatly appreciated.
Not something I can chime in on without seeing you. The decision to keep or extract the tooth is not to be taken lightly.
Hi doctor , I was taking fosamax for 3 years for fibrous dysplasia of bone and then stopped it for 4 months for my wisdom tooth extraction. Now it’s been one whole month after the surgery . When can I start again taking fosamax again ?
likely ok to start up again!
Hi, I have been taking fosamax for 2.5 years now for osteopenia. I want to get dental implants in lower and upper jaw. Can I safely do that if I stop the fosamax? If so how long do I need to be off it?
This depends on many many factors beyond just how long you were on a certain medication. The difficulty of the surgery, other medical comorbidities you might have such as extended steroid use can make you at greater risk. A blood test called the CTX can be done which can give you a numerical value for your doctor to follow.
Hi Dr. Amin,
I’m 72 yrs old I had taken fosomax for 7yrs and had stop for 5 yrs now. My dentist told me that all my upper teeth can’t be saved, and he can put 4 implants and have denture with metal on top. I had bone density test last year and showed that my osteophina is not recovered 100%. I live in the Bay Area but I want to make an appointment with you. Please let me know how long is the process and how much is the approximate expenses. I like the illustration on full ach implants.
Thank you,
Adela Sison
Hi Adela,
It aould be best to CALL the office if your considering having me treat you. I fixed bridge is ALWAYS possible in my hands. We will talk extensively about your bone density. There are many SAFE work arounds.
818-538-5718
I have many patients that travel.
😉
Hi Dr. Amin,
I’m 72 years old, I had taken fosomax for 7 years and stop for 5 years now. I need 4 implants on the upper jaw like the clear choice ad, and had bone density test last year and shows I havent’t recovered 100% from osteophina. Can you please advice if this is a good decision or just have denture? I live in Northern Ca.
I just replied to your other post. All on Four is not great on the upper jaw UNLESS you are using a zygomatic implant.
Hi i was taken actonel for 5 or 6 years , now I;m taken prolia for 2 years , I need 2 extration then implants, what
can I do in this case also the dentist told me I need to have 150 blood results in my ctx test , if i dont have
150 what can i do?
Talk to your MD about a “drug holiday” especially if this is for your lower jaw.
My dentist did a bone graft knowing I was taking Nexium and Boniva w/o giving me this blood test. When he went to put in the peg for the implant the peg fell out within a month (an extremely painful month). Once everything healed we decided to try again. Yesterday he again did a bone graft. He gave me antibiotics and a pain killer. I called my pharmacist to see if I should stop the Nexium due to the antibiotics and she was the first person to mention this issue with Boniva and bone grafts. I am afraid this graft won’t take either and I’m wondering what I can do to increase the chance that the bone graft will work and how I can respectfully question my dentist as to if he knew of this blood test and connection. Thanks for any professional insight and advice. R Hordies.
How long have you been on fosamax and what is your age? Do you take any other meds?
Thank you for responding. I have been on Boniva two years or so. I am 58. I take Excedrin several times a week for migraines. R. Hordies
Dr Amin, I was taking 150 mg of Boniva per month. I stopped 5 months ago because I need a gum flap and graft. Is 6 months enough time off the medication or should I wait longer. Should I even do the surgery I was taking the medication for 2 years
just have your dentist run a CTX blood test on you at the minimum
Dr. Amin, I cannot thank you enough for ALL your knowledge, expertise & wisdom and willingness to share that with all of us who come across your website. It is not possible for me to go to CA to see you but I so appreciate everything you have to say. You make me feel better about this procedure (and I am terrified of it). I hate dental work and I am now paying the price for not being diligent enough over the years. Thank you so much! God bless you!
The bone graft issue is worrisome to me. I have been told that the bones come from cadavers. A friend of mine told me this morning that his friend had bone graft & implants done and she died because of some disease that was in the bone that was used to graft. EGAD! This is terrible! How can anyone ever be certain that they are safe with this stuff?????
The bone that I use is completely dead. There has been no evidence of disease transmission… Ever. Unlike a transplant which is alive, cadaver graft tissue is dead. It must be processed and procured correctly. I use a tissue bank for the last 17 years that maintains extremely high standard. I do not stray from this.
The Bank makes every effort to ensure that each allograft is as safe and risk-free as possible. Extensive medical screening of all donated tissue is done. All medical testing recommended by the FDA and American Association of Tissue Banks, (AATB), is performed on each graft. All tests must be negative before the tissues are released for transplant. There has never been a reported case of infectious disease transmission from an allograft that was processed using the procedure followed by the Bank.
Sterilization Policy
All allograft are to be aseptically procured and surgically removed in an aseptic environment. Before final processing, the allograft is preserved at –70 degrees Centigrade. Once processed, allograft remain in a frozen state until they are irradiated from a Cobalt 60 source with between 2.5 and 3.8 Megarads of irradiation.
• irradiation protocol exceeds our validated Sterility Assurance Level of 1.9 Megarads of irradiation.
• The current American Association of Tissue Banks recommendation for irradiation sterilization is 1.5 Megarads or greater. (D2.500)
• Written verification that the sterilization parameters have been achieved is to be maintained in the donor file. (D2.500)
• Written verification of the sterility cultures for each donor are to be maintained in the donor file. (B2.151)
Dear doctor
I am a dentist and I Had a patient 3 weeks ago. After extraction of second molar of mandible for her , I placed two implants for first and second molar.I had used bone graft and membrane for both of them and then I had sutured the site. Unfortunatly , now my patient suffer from pain and after 3 weeks she told me that she had forgatten telling me about her fosomax! She has had fosomax for a bout 6 month . What is the next step for my treatment and how can I manage her pain?
6 months of fosamax is minimal. Continue to monitor healing with weekly follow auto and X-rays.
I had a LeFort operation, in which bone from my hip was grafted to my maxilla. The bone didn’t take, and both the bone and metal plates had to be removed. I was told that the bone had become infected. I now have less bone than I did before. I can’t use implants and my denture come out as soon as I begin speaking. I had taken Fozimax for osteopenia for about 5 years, but was never asked by the doctor or in the questionnaire I filled out if I had used a bone density medication. So I was not able to make an informed decision. The agony has not ended and it’s been 9 months since the operation.
From a bone loss standpoint you may want to consider the zygomatic dental implant procedure. These dental implants engaged your cheek bones through the mouth and work very well in skilled hands. Some basic testing for residual Fosamax with a CTX can help you determine your risk factors for developing osteonecrosis. There is always an answer!
I have been off Fosamax for 9 months and on the first of the 10th month had a dental implant in my lower jaw. After 5 weeks it has failed. Can this be because of the Fosamax? If so how will know when it’s out of my system?
There are so many reasons a dental implant can fail. What you mention is just one of them. Bone quality, volume, practitioner experience, type of gum tissue, etc. etc. can all be factors in failure.
Usually a CTX blood test would help you to find out. This should be done before having the first implant.
Dear Dr. Amin, DDS
A Conundrum – (thank you in advance for any comments)
Problem, she bites down overnight and her upper gums/mouth… are very sore.
My mom is 92 and in a nursing home. Her front lower 8 teeth are failing (a few are loose the other really don’t serve a purpose and they are sharp) the xrays showed there is no infection. She no longer has teeth on top and won’t wear dentures. We are considering pulling all the teeth on the bottom?
She won’t tolerate a mouth guard, (she’s quite nervous and we won’t get new dentures).
Conundrum II: She took a BONIVA pill once a month for 2 1/2 years, from 8/06 stopped in 2/09. O oh:(
The nursing home wants to do a CTX test, but I’m not sure we should go through with it, requires fasting?!
She has good appetite and her health is fair but is confined to a wheelchair. I give her lunch every day, she eats soft foods.
I, daughter, am beside myself as to what to do.
Thank you very much if you take the time to answer. Thank You!
Trudy
P.S. – As long as the roots don’t get infected, maybe we should just leave them alone and hope the come loose?!
since she discontinued in 2009, she is unlikely to have a problem. The chance of developing osteonecrosis secondary to Boniva treatment at this point has decreased significantly. If she takes steroids such as prednisone for a long time that could increase her risk but it sounds like she doesn’t. If there aren’t any other medical complexities your likely okay to remove the teeth and not likely to develop the complication.
Dear Doctor
If I were living in California I would call in for a consultation but I am living im England.
I would greatly appreciate your opinion on the following.
I am 66 year old male who had a first impant (UL 4 ) in August 2009 and a second implant (UL 2)
in Jan 2011. Subsequently (March 2015) I was diagnosed with osteopororsis and started taking bisphosphonates November 2015, orally. After several months, starting April 2016, I occasionally
experienced a brief sharp pain in the area above the implants; approximately every 2 or 3 weeks.
My thoughts were that there was some reaction happening between the implants and the bisphosphonates.
In your opinion is this likely to settle down or would some investigation (more x-rays) be needed ?
Many thanks in advance.
I would take some more x-rays at this point just to double check everything. The fact that you have osteoporosis means you are losing more bone than you are making every day. Your bone changes every single day and that is necessary for the health and function of your dental implants and natural teeth. Most people do not have problems if they take bisphosphonates after implants have already been there and healed in the years past.
Dear Doctor
I live in England i am 63yrs old I been on actonel and bonviva from 2001to2010 I have since been on calcium and vitamin D supplements 1in a morning and 1at night for the last 5yrs.I have a loose tooth (been loose for last 18months)also some bone loss in upper left and lower right back teeth when I had a full mouth x Ray done.My dentist seems to think I should be ok to have it out because I have been off them for 5 yrs he has never offered any of the blood tests you speak about (what are these tests called and what would I ask for).I have tried speaking to my doctor but she just says it’s a dental problem . I am at my wits end in trying to do the right thing.I was not informed of these problems when I was put on the medication .My doctor is wanting to put me back on them I am classed as borderline osteoporosis ,but I am not sure I want to go back on them .Is there anything else I could take without these side affects .I would truly appreciate your opinion on this thank you .yours sincerely Linda Morrison
after being off the medications for 5 years your risk is reduced. This is especially true because you took only oral medications rather than intravenous medications. Talk to your dentist about this but you should likely be okay.
Dear Dr. Amin,
I’m in Maryland or I would come to see you. I’m 69 years old and in very good health but I had osteoporosis because of an overactive parathyroid, which was removed 8 months ago and my PTH is normal. I have been taking alendronate once a week for 1 year. I know that’s not a lot compared to some, but I still see dentists at drbicuspid.com etc. saying that someone in my shoes should “limit implants”, which I guess means, Don’t have them at all. But I need lower-jaw extractions and if possible, implants.
I didn’t even know about CTX until I read your webpage. I wanted to take your advice about determining if I’m at low, medium or high risk for BRONJ.
I stopped taking the alendronate two weeks ago. (I haven’t fallen in years.)
Before I start the dental work I would like to get a serum-CTX test this week, and again 30 and 60 (and 90? and longer?) days from now, until my CTX is over 150pg or ???pg, or whatever you say I can hope for?
Your answer to one patient in this thread, with Fosamax for 10 years, recommends also testing for bone turnover markers. Should I do that too, and what do I ask for? There seem to be a lot of names for that. And what are acceptable values for bone turnover markers?
Thank you so much for any help you can give me. Without you, I’d know nothing about CTX.
Sincerely, Mike Moran
Thank you for your very kind words.
I would retest her CTX no earlier than 90 days. 30 days is far too early for there to be a significant change. Once you enter the safe zone you have a lower chance of having a problem. The higher the number a better.
Bone turnover markers will test your ability to make bone which is extremely important. The CTX does not do that. There are test that can be done such as a bone specific alkaline phosphatase which can be helpful. The main thing is that your dentist knows how to interpret these. Just because you have the test and it is normal, it needs to be related to other things such as the CTX and other osteoporosis related measuring systems. One test does not do it all.
The NTX is another good marker which is similar to the CTX.
It is a good thing that you know about parathyroid.
Using your own blood platelet concentrates such as L PRF and PRP will also help. Having intravenous sedation with intravenous steroids will also help you heal. There is more to good results and avoiding Fosamax complications than just CTX values.
Very respectfully,
Ramsey Amin DDS
Dear Dr. Amin, Would answer two questions for me if possible, I have been taking fosamax for 10 years. According to your article, I have no chance of having dental implant. Is that a correct conclusion? If I do want dental implant in case, is mini dental implant a safer and valid procedure for patient with both upper and lower denture?
Hello Alex,
That is an incorrect conclusion.
Just because you have taken a bisphosphonate call Fosamax for 10 years does not eliminate your chance of having a dental implant. Mini dental implants are not advised…. They bend, break and I really consider them temporary. Should have standard, normal diameter implants placed.
2 or 3 values from a simple blood test can determine whether or not you are low, medium or high risk for developing osteonecrosis of the jaw secondary to bisphosphonate use. Not only should a CTX be done but also bone turnover markers should be measured to make sure you will grow bone.
Lower jaw always carries more risk than the upper jaw. You can also take a drug holiday and switch to a different type of medication such as Forteo if you need to really be on Fosamax for 10 years or more. Most people that have been on this medication for 2-4 years were taken off because the drug lasts 10-15 years inside of the system. That begs the question, why continue to take it? I suggest you speak to your medical doctor and a really good implant doc.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I took Fosamas 21/2 years, Boniva, Actonel and Reclast (IV). My bones are becoming brittle and my teeth have loosened. Now my four front teeth need to be extracted. I am very feared of ONJ. When I go to the dentist and he measures some of my teeth are measuring 11 and are now to the severe stage. I have been off meds for 41/2 years, but I am scared to have teeth pulled.
You did not mention of whether these are upper teeth are lower teeth. Typically the upper teeth have less chance of developing this complication.
I have 3 atraumatic compression fractures in my thoracic and lumbar spine, my bone density in October revealed osteopenia. I already had a fixed lower jaw bridge implant done 4 years ago.I was planning on getting upper dental implants, the dilemma is per my endocrinologist, orthopedist and pcp all feel I need to take a biophosphate can theses implants be safely done?
Do the dental work first before going on the medications if possible. But keep in mind if your osteoporosis is severe this may inhibit your ability to heal after dental implants in the upper jaw. It is a double edged sword.
I sure need some help. I was on boniva for 8 years then was switched to generic one. I went off it last april 2014 because I have a very painful tooth to be extracted.how soon willi be able to extract the tooth, please help
There is no way that I can answer this for you without some blood tests. Your dentist needs to evaluate your risk for developing osteonecrosis of the jaw from taking Boniva. These medications are called bisphosphonates. There are also other medications that act like a bisphosphonates such as Prolia which can have the same affect.
There are blood test available that I can tell you your risk for developing osteonecrosis. There are also blood test available to know how you breakdown bone and how you build bone. This is more involved than just taking a CTX blood test. This is especially important for your lower jaw and especially important if you have been on these medications for a long time.
If you are my family member, all of these tests would be run before doing any treatment. There are very simple, fast and inexpensive. The main thing is that your safe. You do not want to have this horrible complication which can lead to losing part of your jawbone even.
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
How long before having 8 teeth pulled do you need to stop taking fosamax?
Hello Renee,
There is no way that I can answer this for you without some blood tests. Your dentist needs to evaluate your risk for developing osteonecrosis of the jaw from taking oral Fosamax. These medications are called bisphosphonates. There are also other medications that act like a bisphosphonates such as Prolia which can have the same affect.
There are blood test available that I can tell you your risk for developing osteonecrosis. There are also blood test available to know how you breakdown bone and how you build bone. This is more involved than just taking a CTX blood test. This is especially important for your lower jaw and especially important if you have been on these medications for a long time.
If you are my family member, all of these tests would be run before doing any treatment. There are very simple, fast and inexpensive. The main thing is that your safe. You do not want to have this horrible complication which can lead to losing part of your jawbone even.
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
One of my teeth needs gum grafting. I saw a specialist for gum grafting and was told of some of the risks. I took boniva two years ago, got off for a while and went back on it three months ago. All together I took it 18 months. I am 69 years old, in excellent health and 4 cleanings a year. I am petrified and don’t know what to do. Any advice is greatly appreciated.
Erika Stellato
if you are petrified go ahead and take some of the blood tests that I have suggested to others in other comments. This would be test like the CTX, NTX and bone specific markers.
how long after dental implants can a patient go back on fosamax?
Hello Doctor,
I would suggest waiting 3-4 months. Get a new DEXA bone scan and bone turnover markers to determine is going back on Fosamax is even needed!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I had bone graft and dental implants 4 years ago. Now have been perscribed Risedronate to prevent future bone loss . Can I safely take it or will it cause a problem with existing implants?
It should not be a problem. It is a good thing it had the implants done already.
It is only a problem if you need surgery. Once the implants are placed, everything is fine
hi d-r.I have patient who take biofosfonate.UPPER jaw is anodotia ad i want to put 6 implants.lower jaw have 4 upper teeth and i want to be extract and then put 4 implants .Do patient stop with medication and how long after the operation ..tnx a lot
This is a big question. Are you a doctor?? Have I trained you before??