If you have a root canal and now need a dental implant there are some very important issues to be aware of. This is especially important if the tooth to be extracted is in the upper front area. It will have consequences on the final result and cosmetic appearance of the implant.
A previous failed root canal can be a major detriment to having an implant. The problem is related to a hole that develops in your bone which dissolves the very thin outer wall of bone.
Do Root Canals Work?
Although root canals work, they are not 100% effective. Some teeth may not respond as expected to the root canal therapy. Sometimes, it is clear from the beginning that the root canal is not working as planned. Other times, it may be years later that a problem arises.
The problem is usually re-infection of the root canal or a broken, fractured root. This usually shows up as a painful pimple on your gums.
Often times a root canal is “re-done” if the root becomes re-infected. I have seen patients that have had the same root canal done 2-5 times before finally extracting the tooth and having a dental implant!
The infection causes bone loss to occur around the root where you would need bone for a dental implant.
What is An Apicoectomy?
An apicoectomy, or “reverse root canal,” is sometimes done as a last ditch effort to save an almost hopeless tooth with a root canal. It does not have a very high long-term documented success rate. You have about a 40% chance of losing the tooth in 5 years.
The Procedure: Surgical access is made through the bone, and the tip or apex of the root can then usually be seen through this “window” in the bone. The tip of the root is cut off, and a sealing filling is placed at the end of the root.
Examples:
That is where the problem occurs. The hole made in the bone to do the procedure does not always heal leaving a defect under your nose if it is in the upper front.
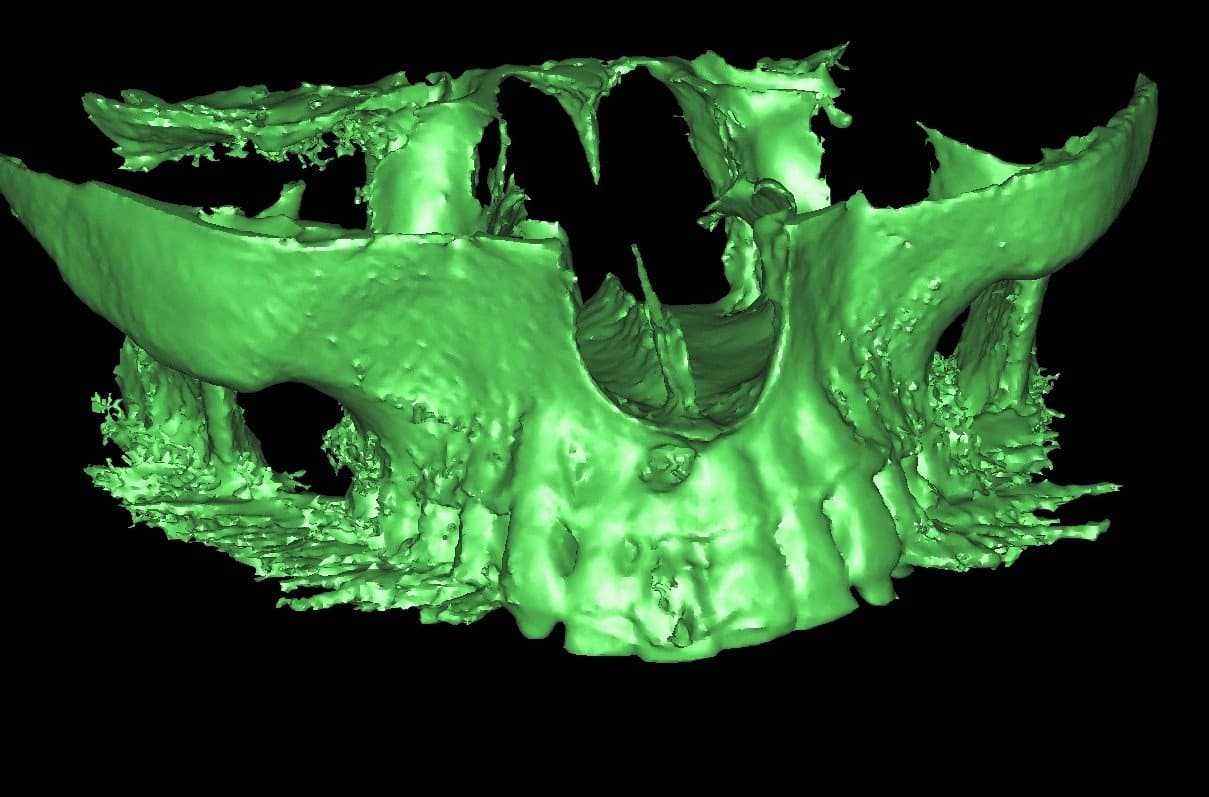
This CT scan image of my patient that I treated in my office in Burbank shows this exactly:
Although, this hole is correctable, it usually requires a more extensive bone graft to correct. This increases the cost and time to have the dental implant.
The worst case scenario is where the “apico” fails and the entire outer bone wall is lost. This usually requires and onlay block type bone graft taken from your chin or the side of your jaw to correct. The block can also be taken from cadaver bone also.
My recommendations…look at all your options and plan for the long-term. Saving a hopeless tooth may in fact be more problematic and costly than extracting and maybe having a same day immediate implant.
Please feel free to comment or ask questions in the comments section below.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Burbank, California
https://www.burbankdentalimplants.com

Dear Dr. Amin,
I am also reaching out to you for advice on a complicated dental/neurological issue.
To summarize very briefly:
– About 4 years ago, my right central upper incisor became painful, or actually the root. I had mostly pain around my right nostril.
– I seeked several opinions from various dentists and finally opted for a root canal, although they could not see anything on the x-ray… Still regret this decision to this day.
– A couple of months after this root canal, I was diagnosed with trigeminal neuralgia. I took anti-epileptic for a couple of years, until someone advised me to try local anti-inflammatory remedies.
– During the last few years, I would put a mixture of camomile (essentials oils, infusion, mouth wash etc.) around the root of this tooth, directly inside my mouth. Everytime my neuralgia would start again, I would do this and the pain would decrease little by little until there was none.
– However, the tooth remained painful when pressure was applied on it. I was not able to bite on it or touch it, without risking to trigger my neuralgia.
– Finally, a dentist found out this year thanks to an HD 3D Scan of the root that some root canal filling went outside the tooth and into the bone. He proposed to remove the excess and to perform an apicoectomy on this tooth, to remove all possible source of inflammation.
– I followed is suggestion. Apicoectomy was performed about 3 weeks ago. I also had a small bone graft.
At this time, my tooth is still tender when I touch it, painful, but not massively when I put pressure on it. However, I have pain around my nostrils and on the sides of my nose. Sometimes it goes up to my forehead, just above the eyes. The pain is very much located around the nose (it has always been mostly located around the nose, even if before the pain would be more widespread on the right side of the face).
Is it normal for the tooth to be tender 3 weeks after the apicoectomy?
How long should I wait before saying it was a failure?
Would you say that it is likely the nasopalatin nerve or the infraorbital nerve that is likely causing the problem?
What couse of action would you suggest to treat this residual pain around my nose?
Thank you very much in advance for your opinion on the subject.
Best regards,
Marie Anne
Have you seen a facial pain specialist at a local dental school? Trigeminal neuralgia is often times overdiagnosed when it truly is not that.
I’m honestly not sure if this thread is still being used.
So I had a root canal for the upper right molar, the one two teeth away from the canine, on December 30 of 2021. For a couple weeks after the procedure, I felt no pain and no symptoms. After that gradually the symptoms gradually returned, those that were there before the procedure.
Most of the symptoms have been on the right side of my head and face. Symptoms such as; nostrils being effected, neck feeling strange, ear having pain and feeling weird, face having spots of numbness and tickling sensations, right eye feeling strange and occasionally painful, migraines, pressure on the front of my head, lightheadedness, episodes of confusion and unable to think straight nor form cognitive thoughts, slight memory loss. All of which I presume the root canal tooth to be the source of.
After reading quite a few of these comments, I doubt the cost and effectiveness of an apeco is going to do anything beneficial for the occasional symptoms. I’m hopeful an extraction might be work, though it’s not even been a month since the operation.
I fear I’m being too impatient in considering “waiting for it to heal”. I fear in being too patient because waiting may not provide the loss of symptoms of that tooth.
The two surrounding molars have infection as well which confuses my dentist as to what’s causing the symptoms. Hoping to get work done on the two to narrow down the cause of the “pain”.
Strange, considering the trigeminal nerve of that tooth was supposedly severed in the root canal, yet I still feel that tooth, or at least the base of the root of it. Then again, that particular trigeminal nerve shares sensations with the two surrounding molars, as my dentist tells me.
As for the symptoms, I take occasional ibuprofen and Tylenol for the pain, valerian root to keep my mind calm and reduce anxiety, occasional benzocaine on the gums to reduce the symptoms caused by the tooth.
I fear the only option I have is to learn to live with it.
I fear the symptoms getting worse with treatment on that tooth.
Is jumping to a sudden operation for one tooth too reckless?
Is waiting too long likely to decrease the success rate to treat it?
What is the success rate of an apaco and of a tooth extraction?
I would see a very skilled root canal specialist endodontist and have a CBCT scan done. None of what you described is normal.
Perhaps one or more teeth need extraction and or a better root canal
Yes this thread is still active! It is one of the best on the site!
😇
Hello, I had to get an apical done on tooth #3. They also did a root canal on #2. After roughly 3 months I started feeling numbness around my head.. It had lasted till present day.. The Endo told me it had nothing to do with the apical.. Then after 5 months or so after the first apical I needed up with an abscess about both those teeth. I went back and the endo told me he needed to do an apical on #3 again. While getting that done he decided to do an apical on #2 also. After roughly 10 days I started to get a headache. Now almost 2 weeks after 1st sign of headache it’s getting worse and worse everyday. My head is all numb and the headache is severe. I can barely focus at times. I had a CT scan done and it came up negative. I’m waiting on blood work results now. Any thoughts as to what it could be? Thank you in advance!
Wow. Something is not right. Are these your front teeth and you are using the international numbering system?
If this is truly #2 and 3 molars you may want to consider extraction.
In desperate need of advice. I had an injury to tooth 8 upper front right it was pushed in and I pushed it back out myself immediately. Went to dentist had x-ray and everything looked ok..fast forward to last year. I went to dentist because serious pain.. she did not have scan equipment so got referred. Scans were blurry so I asked dentist to refer to Endo. Endo did root canal in May. He said my regular dentist would have to do the filling on back of tooth. Pain did not go away two weeks later so dentist didn’t do filling. Went back to Endo he said maybe the root was close to surface of bone and maybe apic needed..sent for more scans and he said root didn’t look close to surface but apic was next step. (Back of tooth still not filled at this point). Six weeks ago did Apic. Large incision from above tooth 9 all the way to tooth 4. He said the root tip wasn’t really that affected. Pain way way worse now just by line of right nostril and sore to press under eye. Tooth is slightly different position now and painful. Twitching in lower eye area, pain in ears and face. Area where Apic was done is so painful when I smile or touch it. Went back he tells me nothing more he can do except refer me to a pain specialist. Family dentist does x ray and there is a gap in the filling (Cotton)? At bottom of root canal near where the hole was drilled to do original root canal and possibly tiny gap near where Apic was done. Been off and on antibiotics so many times now. Now family dentist wants to put me on another week of antibiotics and close hole in back of tooth. I am so upset and frustrated and in so much pain. I don’t know if any of this is typical or normal?
Twitching in lower eye area, pain in ears and face is not normal at all. I would go ahead and see another endodontist and get their opinion. It sounds like you may need to see the facial pain specialist. This should be ruled out before the worse case scenario of having to extract one or both teeth
I hear ya, I’m dealing with the same issue
Wow Ramsey! Finally some information about the infamous HOLE that is left! Thank you! I wish my dentist had made me aware of the pitfalls of this procedure like your great Blog has done… I have had two Apico’s which has left me with chronic (yet minor) cheek swelling and tenderness around the incision site, (upper right molar). In hindsight I wish I had removed the tooth but here we are over two years later and it is still bothering me… Please Can you expand on the hole healing process and wether it will ultimately heal? I also do worry about potential nerve damage. Also how long it takes for bone to grow in around the root? I am now in two minds wether to wait it out, or have it removed.
Again, thank you for sharing this invaluable information and recommendation!
P.s. I have found wearing a tooth guard at night has really reduced the symptoms of swelling and tenderness.
Thanks again!
Ben Fox
Thank you for your kind words. I would have the white check for fremitus. This means that the tooth is moving slightly when you bite down hard. After the bite is 100% adjusted by a really good dentist give it a year before making any decisions. Without seeing any x-rays or examining you I can’t tell you exactly
Hello. I am 25 years old and am currently in a situation that has left several specialists at a loss. About 2 years ago I got a three-piece dental bridge (front left tooth, incisor, and canine) because the particular dentist I originally saw for an incisor implant told me an implant was not possible due to the roots of my teeth being too close together. He told me the only option I had was to go through with the dental bridge, so that is what I did. I very much regret not getting a second opinion on this. Due to several cosmetic issues with this dentist’s bridge, I chose to see a different dentist and have the bridge replaced with a full porcelain bridge rather than the porcelain fused to metal. After receiving this new bridge, my front tooth became sensitive and needed a root canal. After having a root canal done on the front tooth, the canine also became sensitive and needed a root canal as well. After having a root canal done on the canine, there was an immense pain that resulted immediately after. The pain extended from the dental bridge area, down my neck, shoulder, and arm. The root canal was repeated on the canine after a couple of weeks had passed with no change, but no relief resulted. I was then referred to a root canal specialist, where X-rays showed no abnormalities or anything to be worried about. The root canal specialist advised me to instead have an apicoectomy rather than repeat root canals again. I then saw an oral surgeon and the apicoectomy was done on both the front and canine tooth and once again no relief resulted. I was then referred to a neurologist to seek medication to help relieve the pain. I then tried two or three different prescribed medications and again had no relief. I am still struggling with this pain today and no one really has any idea what could be causing it or what to do to treat it. I am at a point where I want to extract the canine out of desperation for relief, but my dentist is hesitant to do so as she feels it might not yield any relief, especially given that the pain extends to my neck, shoulder, and arm, and due to the cosmetic process and general complications that could result from having an implant done. The source of the pain seems to radiate where my dental bridge is, and if I breathe in cold air, it isn’t sensitive, but I can feel it trigger the deep ache in my neck and arm almost every time. I can also feel the deep pain when I poke or press around the bridge area, and this is why I am currently so set on having it extracted. The pain has been absolutely exhausting and there is not a single day where I do not feel it. Do you have any advice on what could be the cause of this and if extraction is a wise choice? Or, are there any other types of options I should be considering going forward?
I am really sorry that you are going through all of this. It is quite possible you have pain of none dental origin we call atypical dental pain. You may want to see a dental pain clinic with in a local university dental school. It is possible you may have trigeminal neuralgia. Sometimes these are treated with medications and steroids and often can be relieved without continuing to do procedures in the area that are not likely to help. Likely all of the work you had done was well done but unbeknownst to everyone it created a trigger. I would not extract anything until you have seen a pain clinic specific to dentistry at a local major dental university. There are people that specifically specialize in this. Around my area of both USC and UCLA have people like this.
Please keep me posted and I hope this resolves for you quickly. 😊🙏
Hi Dr,
I am 34 year old Mom .
I got 2 apicetony one at age of 12 and other at 16. My 2 tooth were bridged . They are uppet front ones
But gum bone stikl shows lost.
The. After the bridge fall out. Dr did brige on other 2 teeth . Now due to cavity and accidentally i chew the fork i lost 4 of them now.
Front upper teeth are gone.x reay showing area without bone also shows additional area being infected.
Now what should i do .
Dr saod we will do impant after you meet oral surgeon.
I am afraid if impants fail then ?
Wanted to know your comments
Based on what you’ve described, I would recommend considering a canine-to-canine bridge rather than implants. The advantage of this approach is that it doesn’t require bone for support and therefore can be a good option given the bone loss you’ve experienced. This bridge would anchor on your canines and span across the gap, replacing the lost teeth without the need for implant surgery.
Doctor thank you for your help. I have an infection in my crown [back upper left, 14th I believe] and the dentist recommends the graft and implant. Is that initially too aggressive? Should I try the apico first? Thank you so much.
Read this article as well
https://burbankdentalimplants.com/infected-root-canals-molar-implants/
manufacturer of API
Hi Doctor,
Thank you for sharing your knowledge to all of us who are scared and worried about our dental concerns.
I have many issues, cross bite, tmj, tinnitus, and neraglia and many crowns and root canals.So I have a pretty high tolerance to face and dental issues. I recently had a re treat on #9 root canal and afterwards it was still causing pain so I proceeded with the apico, it has been about 4 weeks, after the surgery which I believe was quite invasive and I have been through many processes, I have had pain in my bottom teeth and pressure on my tooth with procedure and sinus and nose area. The pain in the bottom teeth radiated because she said it was due to cutting near nerves for the procedures on the top tooth, I was placed on antibiotics and pred. I presently still have pressure pain and numbness above and on the tooth and sinus area and my teeth on the top and bottom get sensitive as they were never like this prior to the procedure. As you said to give it time, do you think I am still in the healing stage.
It is an older root canal tooth and retreat recently and trying to avoid extraction but I have been in pain since last September 2020 and I need to feel relief. I do have two previous implants in molars and did not have any issues. Thank you, Is this just a healing face that I am going through?
After only 4 weeks I would wait longer. Give it 12 weeks. If no improvement, have a same day implant.
Thank you Dr. Amin for your follow up . I appreciate your time and expertise.
😊
So sorry to hear what your going through. I have had root canals that did not settle and Apico was offered, fortunately I did not go through with it. I also have neuralgia. I feel if I had done that it would have been the straw that broke the camels back. There are so many nerves in there. Can you take b12 and other things to help calm your nerve endings to allow them to heal? Maybe your doctor can perscribe gabapentin to help calm the nerve irritation?
Thank you Dr. Amin for your expeditious follow up, hopefully the tooth heals.
I am very happy to have found your sight and for your dedication to your profession.
Hello,
I’m a 25-years old female. About 10 years ago I had an apicoectomy on my front tooth. After the operation, my pain went away but my tooth was always sensitive. I never bite or chew food with my front tooth, I’m always careful because it’s very prone to pain. Recently it has gotten even more sensitive. I constantly have dull pain in my tooth, so I was hoping for a dental implant. However, because of the apical surgery there’s a bone loss, so my dentist thinks that a dental implant is not possible.
Since it is my front tooth, I’m very nervous about extracting it, then the dental implant fails and it will be empty. I’m never comfortable with my tooth, I’m always scared.
I want a dental implant but scared that it won’t work out. I’d appreciate it a lot if you could give me an idea about what to do.
Thank you in advance.
At your young age I agree this has to be done very well. It would be very rare for me to not be able to replace your front tooth. Perhaps find an expert DDS and do a second consult. I have done many single center implants on young ladies your age after apicos!
Watch the video on the link above
I am 28 years old and had to extracted my upper molar #14 due to a failed root canal I was wondering if an implant would be a good option for me . I struggle to eat and chew everyday cause of the missing molar.
Yes it is generally the best option for most patients!
Hi. Over 30 years ago I had a lot an apicoectomy on my upper front right – central right incisor – (having broken it as a young teenager, having it capped, then eventually crowned when my mouth matured). A few weeks ago an infection developed for which I was prescribed a course of antibiotics. Xrays were taken and it has been recommended that I have another apicoectomy. The infection has cleared though it does feel a little different (no pain, just slight numb-type sensation). I am nervous about another invasive procedure, given the history of the tooth/root canal and am reluctant to go ahead now that it seems to have settled. Would I be foolish to leave it alone for the time being?
Waiting is not going to help it if it has symptoms 😥
Hi Doctor,
I would like to know your opinion on my case. I got a root canal 2 years ago on upper tooth N.12. Last year I started having issues with that tooth and I got an apicoectomy in September 2020. At the same time I started with Invisalign the same month. The apicoectomy failed and I got a new one in December 2020. Once again I am having issues with that tooth, there is a small fistula, it hurts sometimes. My dentist has told me that we need to extract that tooth and after I am done with Invisalign I will get an implant. I will be done with Invisalign in 4 months. Should I get extracted that tooth while on Invisalign? It wouldn´t be better to wait for the extraction? Are there any chances of saving that tooth?
Many thanks in advance
Not many chances of saving that tooth if it’s been done twice already.
In my practice I would remove and replace the tooth all in a single visit including a bone graft. This is a very advanced technique and not necessarily main stream buying your average dentist.
If they’re going to do staged treatment with extraction first I don’t see any problem in removing it now and doing the bone graft while you are in orthodontics
Dear Dr. Amin, I had an apicoectomy on my lower first molar about a month ago. But the tooth still feels strange, a little sore, not particularly when I chew, just spontaneously. Does that mean that there is still some infection, or it is just healing slowly? When can I expect it to feel “normal” (or nothing) like my other teeth? This tooth had a root filling many years ago which apparently failed, this is why I needed an apicoectomy instead of extraction.
Appreciate your response!
This type of procedure takes a long time to heal. Give it several months and see how it goes.
Hi Dr. – I had an apico and bone graft with an oral surgeon four months ago (on a front tooth with a veneer). Bite was a bit off so dentist filed a tiny bit. Now every time I sneeze the cold air from breathing in shoots up the tooth. How is that possible? Is it likely from the apico or a potential crack from the filing?
Usually that sensation does not last too long. Has not gone away since you posted this comment?
Usually that sensation only lasts a few days.
Hi!!! I had a partial apicoectomy on #14 (I think) 3 weeks ago tomorrow. Previously that tooth had 2 failed root canals. It has never bothered me and I only knew it needed treatment this time because I went in for a broken crown. In the past day or so I feel like that area of gum is still a little swollen…and not painful, but maybe tender…and I have a headache today. Should I be concerned at all? Thanks!
14 in the American 🇺🇸 system is an upper left molar. That is a very difficult tooth 🦷 to do this. Hopefully it works. Give it time
Oh goodness! I didn’t realize it was difficult and wish they would’ve told me. I hope it is OK too…I was just worried that the lingering swelling/tenderness might mean infection or other problem. Thanks for your feedback!
I had a root canal and crown 3 months ago. Yesterday i have pain in the same tooth. XRAYS were taken and unfortunately nothing definitive on where the infection is.
The root canal doctor because i’m 70 suggested i do an implant, which is fine.
If you were my Dentist knowing that the 1st root canal failed, what is your opinion. I don’t care about the cost as much as I care about being pain free.
thanks
Take a CBCT 3d scan to confirm it is not another tooth before it gets pulled!
Hello Doctor!
Also, I have another quick question: I was seeing my dentist yesterday and I’ve been told to do a 4 fillings on upper left #13 & #12 and on the lower left side #13 & #12. The doctor says: she see cavity and decay on these teeth. On all these teeth previously I did fillings been done on the side on the teeth and looks like it needs to be re-done again. I do feel pain on upper teeth, but not on the bottoms. What would be the best advice? What should I do?
Thank you!
Alex
If decay is present, it is best to correct!
Hello Dr., I had an apicoectomy on my right front tooth and it’s been 18 days now since the surgery. I dont feel any pain but there’s like a lump and tightness specially when I say the letter “o”. What bothers me the most is that my right nostril became smaller and my nose appeared bigger. What possibly did go wrong? Will the lump flatten? Will my nose go back to it’s original form? I’m really devastated now. Please let me know what I can do.
Hmm. Give it 6 weeks. If it is just swelling it will go away. Keep me posted. A bit strange.
It’s been a month now and I went back to my dentist because the lump is still there. It’s a hard lump which I think a hard tissue or scar formed. Kinda like a keloid maybe. So he wants me to go back for another procedure and he’ll remove the lump. Do I need to seek a second opinion? I’m scared. What if it get’s worse? 🙁
I would do a second opinion on your case. Why not?
Hi Alyssa, I’m having the same problem with my upper left tooth. I have no pain or anything just the lump bothers me.
May I ask what the outcome of your situation was? The corona situation here is really bad and I don’t want to make another trip to the dentist 🙁
Thanks,
Eithane
Hey guys! This is indeed bizarre- I hope you are both well… I have had 2 Apico and I WISH the dentist had explained the procedure thoroughly. I find it alarming I have a hole in my jaw which according to this article may not heal!? I have a swelling in m cheek for nearly 3 years now- very slight, but I notice it; the area of incision in the gum is also tender when pressed (not painful). I adivise wearing a guard at night – since wearing one the swelling and discomfort is much less- hopefully now it will heal
Alyssa, I’d love to know what happened in your situation. I have a hard lump as well that is sensitive and very annoying but not necessarily painful. I’ve been to many dentists (endodontist, periodontist, TMJ specialist etc) and eventually had the tooth pulled but the lump is still there. Although I do believe it’s gotten smaller… what ended up happening for you? I’d love to have it removed but am scared it’ll cause more problems somehow.
Apicoectomy
Hello Doctor.
I want to say thank you first for allowing an opportunity to discuss dental issues with you in ways like this forum, particularly when the article was from 2010 but you still continue to reply to those of us in these predicaments!
Anyhow, I have an issue with tooth #3 which originally had a root canal preformed around 2011. Unfortunately, during the procedure the dental file broke (which he informed me of) but was left inside. He preformed the remaining root canal and sealed it up, but years later I started to get a “pimple” abcess.
I was told by a separate office that it was going to require a very delicate microscopic procedure to have the file removed and was quoted about 3k to fix and if it didn’t work, I’d then have to pay additionally to have it removed.
Needless to say I had no insurance and let the tooth go for several years until I started to belive it was the cause to the terrible debilitating migraines I was having.
Fast forward I found a new endodontist that was confident the tooth could be saved and that I just needed a retreatment and that would also fix the abcess, so I happily obliged.
After the retreatment I was happy to have the abcess fixed but noticed only about 30% percent improvement in the migraine department so he told me to wait another 6-8 weeks and if I didn’t have full improvement to contact the office again.
Eventually after waiting and still no full recovery, I requested to go ahead with the next recommendation which was to have the Apicoectomy and once and for all attempt to get the file officially removed from root/gums deep inside.
Eventually the api was performed and he was able to get a tiny slivers worth of the file out!
He believed it was most, if not all of the file and I actually got to take the tiny sliver home with me as a souvenir! (yay me) lol.
It was finally then that slowly I noticed my migraines disappearing a little more each day until It came to a halt at about a 50% reduction this time. So now a 30% reduction from the first retreatment and another 50% from the api for a total of 80% fix.
This was great in the beginning until I realized it wasn’t getting any better and in fact seemed to be getting worse again month by month until now I am back to having debilitating migraine to which no medication will work, and my pcp can’t seem to find any reason for them either. Scans preformed etc.
I reached back out to the endos office, it’s about a year later he tells me to come back in we will preform 3d images. We do the scans, in his words it looked great, the procedure went well and he believes my migraines are a result of something else and would not indulge me in any conversation about pulling the tooth or any further instructions really.
So here comes my question, and I apologize for the long drawn out history of the tooth.
But my concern is with pulling the tooth and its history, and wanting to get an implant eventually after.
If I have it extracted, does anything else special have to be done considering it had a previous api? Does that need to be cleared out again too? The Api area?
Do I need to have any special procedures to account for anything that could be left behind from the api, or just a surgical extraction should be good enough?
Truthfully, because I let the tooth go for so long originally, and still have it in my mouth now that I’m worried it actually has a lingering infection somewhere that can’t be seen, hence the migraines. I never had a history of migraine before and neither do my parents.
Any advice on this situation would be greatly appreciated.
Also, I am not an immediate candidate for an implant either because Id have to undergo a sinus lift. (another reason why I didn’t pull sooner).
Thank you so much in advance.
-Chelsea
My email [email protected]
I appreciate the detailed story. If the tooth looks good on x-ray and feels okay I would not pull it out. Migraines have such an unusual etiology. One of my close family members gets them and we still have not figured out why. I would hate to see you remove the tooth and still have the migraines which seem to be your primary concern.
The upper molars typically are embedded into the sinus. Typically and internal or lateral window sinus graft is needed on probably 60% of implants placed for the #3 tooth which is the first molar where the sinus hangs the lowest. Is not likely that any sort of lingering infection is going to cause these migraines. Realistically you may have them for a period of time in your life and then they eventually go away. Imitrex is a great medication for that and can work quickly if you take it fast enough right at the onset of the headaches.
And just because you need a sinus lift does not mean you cannot have any immediate implant. You just need to be seen by somebody who has a higher level of skill and experience. I hope the best for you and stay safe during COVID 19!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
Dear Ramsey,
I would like to know you opinion on socket preservation with PRF at the time of extraction.
I have about 10 mm asymptomatic cyst at upper first molar due to failed root canals and would like to know the best way moving forward. My aim is to make everything possible at the time of extraction to preserve socket and, if possible, avoid sinus lift later.
Would you be so kind to take a look at my CT scan and help me with “non-professional” advise? I’m aware you can not advice professionally online, so just a friendly and legally non-binding tip would much appreciated. Kindly note, I’m well educated in the field.
Kind regards,
Lorem
here you go! PRF! Great stuff! PRF! Great stuff!
Hello Dr,
I have a front tooth that was damaged due to an accident when I was 9yrs old. The tooth gradually went black and I had the a root canal (10 years ago) and then eventually an apicoectomy with a small bone graph (3-4 years ago). It’s starting to now become bothersome. I’ve been told the likelihood of the tooth surviving long term is doubt luck due to the history of trauma. When during the lifeline of this tooth should it be extracted? Is this something that should be done sooner rather than later or Is it best to let nature takes its course? What kind of dentist or specialist is needed for these procedures and how much planning should be considered?
Thanks,
Kirsty
Palmdale, CA
If the tooth is not painful and it looks OK it may be safe to leave it for a while. Each situation is unique. You certainly want to see somebody who has a lot of skill. Replacing a single front tooth is more difficult than any implant in the whole mouth. You kind of need to prepare mentally for its loss. Stay safe during COVID-19
I had a deep root canal on one of my front teeth a few years ago. In August of last year I did an api as it became abcessed. It is now May and I have what seems to be another abscess. The other issue is I am currently 7 weeks pregnant. I am wondering what the best procedure would be moving forward and if I can have an extraction soon. I’m also worried about spread of infection as well.
I had a deep root canal on one of my front teeth a few years ago. In August of last year I did an api as it became abcessed. It is now May and I have what seems to be another abscess. The other issue is I am currently 7 weeks pregnant. I am wondering what the best procedure would be moving forward and if I can have an extraction soon. I’m also worried about spread of infection as well.
Hi Dr Ramsey,
I had apicoectomy done on my upper front tooth 2 years ago. Until now, I can still feel tenderness on the part of my gums near where you indicated the hole is for the surgery.
Other than the tenderness, I have had no pain felt on the said tooth.
Should I be concerned that there is still tenderness or is that normal even after 2 years? Is a bone graft necessary for me or is it okay to leave the hole like that? Thank you.
Unfortunately something is probably wrong. You should have a 3D CBCT taken to check the area. This will allow imaging in all dimensions.
I had a apicoectomy done 4 months ago and my gums are fine no lumps or redness. But i dont know if is just in my head or my tooth slightly moves. What can i do?
Have the DDS check the bite. The root is now shorter than it used to be so there is less holding it in. The having the bite adjusted so that it does not touch is critical to the success especially if it is a front tooth. If it is biting too hard it will cause major problems
Hello i had apicoeptomy done on my froont tooth year ago. Yesterday noticed on the gim redish and white lump looking like absess. Can antibiotics help or do i need to loose tooth.
Antibiotics ‘might’ help. Learn more on this article.
I have had two root canals on tooth 26, one in 2002 and one in 2018. Two weeks ago it was infected, with severe pain.. My dentist prescribed 10 days of Clindsmycin, then an extraction followed by a bridge. He said there is not enough bone for an implant. I am wondering if I should go to an endodonist to see if the tooth could be saved. I am 79 years old.
Thank you.
Going to an endodonist would not be a bad thing. A second set of eyes to examine you.
Hello Dr. Amin
I am a 19 year old from India..Lost 3 of my front upper teeth back in 2012 and had RCT done .
Now infection came back and had dissolved my jaw bone ..Hence had apicoectomy done on the advice of my dentist.
Can it fail ? Do I not have a chance of getting implants in the future?
Yes apicoectomy can fail. At your young age try to keep the teeth if at all possible good make sure your oral hygiene is impeccable and your dental work is done to a very high level.
Stay safe during COVID 19!
Dr Ramsey,
I have a root canal tooth #12 which is failing. #13 was also done however I think that is ok. #12 hurts to bite down on and has never felt quite right since day 1. I was told my options are extraction or apicoectomy. The tooth was retreated twice before the final restoration.
I wonder what the chances are of the apico working or if it would be best to just extract? I was also told 12 had something interesting. He said one of the roots branches out top to my gum and has no bony covering, hence I can feel it when I push on my gum and I also feel pain there.
If I were your patient what might you suggest? I am a healthy middle aged female.
After two root canals I think you’ve done everything that can be done. The chance of successful treatment with apicoectomy is pretty low. Even though the bone may be thin on the outer wall I can typically remove and replace this tooth on the same day and always keep a tooth in the smile! It will require a bone graft and you will not be able to chew on it for 3 to 4 months but at least it will look great! I did two tooth # 12 this week alone! And it’s only Tuesday!
It’s a very predictable area. Make sure you see a skilled and experienced implant dentist as I do consider this a front tooth and it is a bit tricky.
Please help advise needed. I had a old root canal on the bottom left in back. Then it failed and I got a second root canal. Years later had a CT scan that showed it was infected..So I had a apical surgery that failed within 1 month..puss coming out the side of my gums..had it drained….on Keflex 500Mg every 6 hours for 10 days. Is it possible to clear up with the antibiotics? Should he give me a refund? Will I need the tooth removed?
Worried !!!!! Tracy
It sounds like you may need removal of the tooth. It sounds like he had 2 root canals then and apicoectomy which does not leave a lot of tooth behind. A dental implant is a much more predictable procedure than a tooth that has had this much work over the years. Maybe they can credit you some of the money towards the implant but that is not necessarily required.
Thanks for the fast reply. How long should it take the bone to heal untill you can do a implant for me? Also under the CT scan..2 other root canals on the other back side of my mouth are infected..They look perfect on the x ray..only the CT shows it. I need a break and need at least on side to chew on!!!!! How long can I wait to address these? Thanks again Tracy
give it longer than the normal 4 months. I would wait six full months
give it longer than the normal 4 months. I would wait six full months.
I have a severe injury wen I was 7 years old . I had undergone 3 repeated root canal surgeries for same teeth . Then I went through apicoectomy for 3 times .. now it’s almost an year after the previous surgery .. I feel little pain in those teeth again .. iam really fed up with this problem .. those are my front tooth .. I have no idea of what to do … any suggestions??
Implants in the front of the mouth are considered the most difficult. I suggest you see an expert in both the surgical and restorative side. In my hands, this is generally a single procedure to immediately extract, implant and bone graft
Hello Dr. Amin, I recently have begun to experience pain in a tooth (my left side, upper front) that had an apicoectomy procedure done many years ago-about 10 years. I told my new dentist about it and she says it has to be extracted. Is it possibly just an infection that needs antibiotics?
Antibiotics really only provide temporary patch if there is a real problem. I hope to be wrong but it sounds like you might lose this tooth. 🙁
It sounds like you may need removal of the tooth. It sounds like he had 2 root canals then and apicoectomy which does not leave a lot of tooth behind. A dental implant is a much more predictable procedure than a tooth that has had this much work over the years. Maybe they can credit you some of the money towards the implant but that is not necessarily required.n
Hi dr
My endo took a CT scan and told me that the tooth looks really good. I still have a small white gum pimple. He wants me to wait another 4 weeks to see if it will close up on its own. The pimple formed after the apico. Surgery. No pain…he said it’s safe to wait and see for now..your thoughts??
I would give it a chance and re-evaluate after those 4 weeks.
I would give it a chance and re-evaluate after those 4 weeks..
Good morning Dr. Ramsey Amin,
Hello. I’m a 34 year-old woman with pretty decent oral hygiene, my biggest flaw is I’m a floss-a-holic. 😁 I suffer from severe OCD and don’t know when to quit flossing. With that said I have literally flossed my gum line to the point of receding to root exposure. I have already had a root canal in tooth #11 as a child due to an accident which at the age of 17 I had to get an implant because it didn’t take. Last year out of nowhere tooth #9 & #10 started hurting severely just the teeth not the gum line or anything else only when I tapped on the teeth. With x-rays and all there was no cavities no erosion nothing visible to the dentist. They looked further with some 3D x-rays and seen that high up in the route almost to my sinus cavity the route was split and kind of getting infected from tooth ##11 when I was a kid and they probably didn’t see it from the accident, they told me a root canal would not work . The only thing I was able to do was either pull the tooth #9 and cap it as well or get an Apicoectomy,and cap #10. Well being that I did not want to lose the tooth I drove from Wilmington North Carolina to Fayetteville North Carolina and had the procedure done. We are now going almost a year-and-a-half past the procedure and now I am having nothing but trouble with the area. I keep on getting severe infections in where the canal was scraped for the procedure nothing but pain all over again and my dentist wants me to go back and forth to Fayetteville again to try the procedure once more. There is no promising that it’s going to work of course, however, it’s not like I am close to Fayetteville it’s 3 hours there and 3 hours back and also takes 3 days to do each step the post-op the procedure and then removal of the sutures. I totally understand that it’s my tooth was trying to save, however, that’s 3 days missed of school for my three children 3 days missed of work for my husband and I and on top of that almost $100 each day between gas of traveling and breakfast and lunch for the five of us for the day and then the procedure on top of it. Do you think as a second opinion I should try the procedure again or should I try doing the root canal and seeing if a root canal works first b/c that was not done, and nowwould be an option since I had the surgery and it’s the root getting infected not the nerve? Money-wise, it’s going to put a hole in my pocket regardless, or skipping all that pain and sorrow and maybe just doing the implant like I did originally with tooth #11? I know I rambling but it’s a very important deal because it’s my two front teeth were talking so I needed a second opinion and I read all your comments and answers and you seemed very honest and all the people that had written to you seemed very pleased with your answers and very trustworthy to take your opinion. Thank you so much for your time and I’m hoping to hear back from you shortly. With greatest regards,
Cat🦷
Get an opinion from an endodontist. If the tooth is cracked vertically it has no hope for a root canal. If not, there is a good chance it could be saved bby an EXPERT dentist. Prayers!
Get an opinion from an endodontist. If the tooth is cracked vertically it has no hope for a root canal. If not, there is a good chance it could be saved bby an EXPERT dentist. Prayers!!
Tooth number 14 recently had a root canal and also apicectomy the front root. My question is can you also do an apicectomy on the other two roots located in the back?
It is really hard to reach without making a hole in your sinus. 😔
Hello, so I had an apical surgery on my two front teeth three weeks ago but I still feel bump over the surgical area and stiffening discomfort too when I smile. What could be the situation?
Give it more time… At least 6-8 weeks before becoming concerned about infection or failure
I, too, am having sensitivity/pain and a loose tooth after apicoectomy. The doctor stitches my lip to the wrong area of my gums, so I can’t really tell if the “pain” is just whacky nerves or an actual failure
If the tooth is loose there is almost no chance this will take. The tooth must not be mobile so the bone can mend like a broken arm in a cast.
Have your bite adjusted to make the tooth stop 🛑 moving before you can say this is a failure
Hello Dr. Ramsey Amin,
I had an Apicoectomy in the teeth # 7 & 8 on Tuesday 9/3/2019. I had numbness feeling in those teeth for three days and still hard. The problem that I have a sharp pain in the left upper side as muscle and burning around the teeth and today when I drank a hot sweet tea I had a sharp pain in teeth # 12, that spread to 11, 10, and 9 that I took Ibuprofen for it and put heat and ice on my check but the pain come back when I touch and sweet fruit and hot dring and still there. Please let me know what caused the pain fort the upper left side after the Apiectomy of # 7 and 8 teeth.
Many Thanks!
It sounds that the 2 are not related. Generally sweet sensitivity is a sign of a cavity on the tooth that does not have a root canal…yikes!
It sounds that the 2 are not related. Generally sweet sensitivity is a sign of a cavity on the tooth that does not have a root canal…yikes!!
It sounds that the 2 are not related. Generally sweet sensitivity is a sign of a cavity on the tooth that does not have a root canal…yikes!! !
Hi Dr Ramsey,
By reading this, I am very much afraid that this happened to me. I had many problems with my tooth 14. First, a dentist pushed way too strongly to tooth 14 as to replace a filling. It seems she had rage and did hurt me a lot. A trauma to the bone resulted into a major infection that never went away. I was in severe pain and never took any responsibility from her action. Then, I of course lost my tooth before I had two apics. One in the back, the second one. 12 years after the first incident, trauma, infection… I still have pain in that area. Sometimes the pain is really heavy and extremely difficult to deal with, most especially when I am very tired and/or with a strong headache, like yesterday. I still have a hole in that area, we can see clearly, that dark area on top of where was tooth 14. My new dentist will take a scan in two weeks. Can you imagine that my old parodontist never took the time to listen to me when I told him I still had pain in the area where he performed the chirurgy 6 months after his work!! He did not even took an ex-ray! Now after reading this, I am very much afraid that my sinus is affected! As a matter of fact, I have constant mucus that comes out of the cavity. I have such pain, I feel it everywhere on that side, all the way down to tooth 17, up to my nose, up to my cheek and eye… I am so discouraged to live with such a pain… and with no tooth 14! Do you think that one day I will be pain free? I wish so much for that pain to go away. I was butchered… and it affect all my life. Please, help me. Can you tell me what is wrong with me? If the dentist made a hole in my sinus, can this be fixed? Can you tell me if one day, I will be fine, pain free? Sometimes, it is excruciating pain and I don’t see the day when I will be able to eat with my teeth in that area. I appreciate your help and will do as you recommend. Thank you so much and take care.
YES!! –Do you think that one day I will be pain free?
You need to see an ear nose and throat specialist (ENT). Asked to have your sinuses evaluated. If your “ostiomeatal complex” is plugged this will result in pain. Once this is cleared up you can easily have an implant in that area with a sinus lift bone graft. This is an area that is very typical and easy to treat in my office. Your medical insurance will probably cover the visit to the ENT physician
Dear Dr. Amin,
I currently have an infection in the root of tooth #19 (US). Last week I did a round an antibiotic for an abscess along the gumline. The tooth was root canal’d and crowned probably about 15 years ago…
I’ve had 2 opinions from: one was get an apicoectomy and one was to get it pulled. The Dr who suggested the apic said there was a 70% success rate, but it seems from my research that that may be high. My dentist thinks I should do the apic. The emergency dentist I saw last week said get it pulled. The thought of losing my tooth isn’t appealing, but neither is having both done in the next five years. Any advice would be greatly appreciated.
I’m a 44 yr old woman in good health, if that matters.
Thanks!
Apico is good for a tooth with one root. 19 has 2 roots and 3-4 canals. Success is low on molar and access is tough.
Implant likely a better option. Sorry 😐
Dear Dr. Amin,
I am trying to get an opinion on a problem after an apicoectomy I had on March 26, 2019, on tooth #10 (US numbering system). I had problems with the tooth starting in January. The pain was mainly under the ey but radiating into the jaw. My endodontist diagnosed a problem (dark shadow) above the root and noticed that the filling was disintegrating. He retreated the root canal and as this did not help (the exact same pain returned) he did an apicoectomy on March 26. He told me that he found a lot of scar tissue and bone material, which he removed. He added some bone and sutured the thing up. There were no problems until this weekend when I noticed intermittent pain above the tooth (pressure) and the same symptoms (radiating pain upper jaw into the jaw joint). Is this nerves regrowing or indicating that there is something else brewing? There is no swelling, the area above #10 is understandably sensitive. Thanks so much as I am at my wit’s end.
give it time…these heal SLOW….it may take 6 months before you ever know whether this is going to work or not
Hi I Had root canal on my front tooth 17 Years ago. I Had veneers and 1 crown put on my front teeth. The Crowned tooth kept being painful for a year after crown. Went back and the dentist did my crown again. The pain was still there. 3 month ago i went to top endodontist in London and HE redone my root canal through crown saying there is a Tiny bone loss and there was a small infecation near the root.
The pain is still there today 3 months later. Went back to him and 3 other independent dentists and periodontists and they all took x rays saying the root canal has been preformed to top quality and there is no infection there any more. However I am still in lot of pain. It hurts in my nose above that tooth to the point I want to pull it out. At the moment I have been referrered to ENT they looked in my sinuses all normal. I am currently waiting for a sinus scan. I just do not know what to do any more. Have you got clinic in Uk? Thank you
I would not race to remove this tooth or do an apicoectomy unless an endodontist feels that an apicoectomy will help.
I have patient just like you in my practice that wants me to pull her front tooth because she has a similar situation. She has seen neurologists, etc. and nobody can find anything but her tooth still hurts despite everything being perfect. I have never treated her but my biggest concern is that I remove the tooth and the pain still exists… Like a phantom pain
Unfortunately there is no way to know this without removing the tooth.
Hopefully you can get resolution. You should maybe consider seeing a faculty member in a dental school
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi, and thank you so much for your reply. Just an update from me. Sinus scan showed a small bony growth near trigeminal nerve which could be operated however the side effects could be anasteshia dolorosa. I decided not to go for that option. I have been referred to neurologist who prescribed Tegretol. This medication changed my life. Unfortunately I have been diagnosed with suna/sunct, migraines and mri showed brain cyst.
My symptoms changed to Short extremely painful stabbing In right side, blocked nostril,and stinging eye, sometimes red and watery.
Now since Tegretol calmed it down every so often I get a flare in my right tooth which then goes up my nostril and my right eye. They suspect that it might be atypical trigeminal neuralgia or atypical ondologia.
I am writing a diary and I am meant to see my neurologist, but due to COVID it has been delayed.
I will update again once I see neurologist. Just to say thank you so much for your time.
Just a question please, I stumbled across biological dentist who scared me and who said I must not have root canals in my teeth and to remove the tooth ASAP, since it most probably has NICO and cavitation in the bone. I am not sure about this since Tegretol is helping and since 8 different dentists, periodontist endodontist comfirmed they can not see an infection on the scans. Could you please help, I am not a medical person and never heard of Nico and bone cavitations from root canals. Thank you.
I would be interested in seeing the doctors reply to this. I also have root canal teeth that are not quite feeling right and I have been told by numerous health conscious people and even through a forum with bio dentists to pull all root canal teeth. But doesn’t that open the door to potentially more issues?
Hi Dr. Amin,
I recently had an apico done a week ago after having problems with the original root canal on 3 separate occasions. Everyone I called or went back to the dentist I would be told “it’s normal to have pain (3 weeks later) your body is healing still”, or “ it’s not pain from the tooth that we worked on it must be from an adjacent tooth that needs work”, or “it’s just phantom pain”. These things were told to me over a 6 month period. When I did go back the first time to the dentist who performed my root canal he said the X-ray showed nothing wrong and it was normal to have pain still. The second time almost a month and a half later he said he was going to go back in, clean everything and make sure it was ok and that an infection hadn’t occurred. I was in his chair a grand total of 15 minutes. I was a little loopy from the Valium prescribed to be prior to dental work but I know there’s no way a dentist can take off a crown, take a post out and clean everything out and make a new temp crown in 15 minutes. I didn’t know it then but after speaking with a friend who works as a dental assistant I was more educated. Finally almost half a year later the dentist tells me I need an apico and to make an appointment for the oral surgeon in the office ASAP bc it needs to be worked on before I loose the tooth. Reception told me they had no available appointments untitled the new year 2019 and this was in August 2018. They referred me to other specialists, but all had similar wait times. I was going crazy bc of the pain and fear of loosing my incisor tooth. The office that did the work was no help getting me in sooner. Even though they said it needed to happen promptly. Skip ahead to a week ago when I finally got to see the OS he did 2 extractions and the apico in one day. Told me to watch for mild swelling, some pain and not to eat anything hard. My whole mouth was numb for over 24 hours which I was told is normal. Except now the right side from lip to chin where the apico was done is numb still and I can’t speak very well. There’s also an odd smell coming from where the sutures are but the dentist said it’s ok and again “Normal” and not to be worried. He also stated that my lip may remain numb for up to 8 months!!! That doesn’t sound normal to me. I’m worried about nerve damage or damage to the bone/tooth. I am looking to get a second opinion soon. Also the OS who did the apico and extractions can t see me until next month. I just feel like he would have a better understanding of what’s going on than a General dentist considering he specializes in what I had done among other things. And the dentist was not trained for certain things according to the office. Please any advice would be greatly appreciated. Thank you
Hello Dr. Amin, In 2018 I had quite the year with root canals. My dentist performed a root canal on my left canine tooth which had an existing crown. That went well but my front tooth (#9) became sensitive to pressure. No pain, just a sharp sensation when I pressed on the tooth (crown). A root canal was performed on this tooth February 2018. I continued to still feel the sensitivity to pressure for several months. My dentist could not see any indication of infection after many X-rays. Eventually a 3D X-ray was done and a small dark area behind the tooth beside #9 was noted. This tooth also had an existing crown. So a root canal was performed and the crown broke. There was a lot of infection so I was put on an antibiotic and had to wait a week to finish the root canal. I never felt pain or sensitivity in this tooth before the root canal. In the meantime I’m still experiencing pressure sensitivity in tooth #9, so I’m sent to an endodontist who performs a second root canal on the tooth. I’m also put on an antibiotic. The original crown over the tooth was removed as I cracked a portion of it off while eating. So they examined the original tooth and it was not cracked. It’s been five days since the 2nd root canal and I’m still experiencing the same “pressure” sensation which started Feb 2018 and it is now Jan 2019. Do you think I had infection in the general area (front) and somehow all three teeth were infected? Prior to this I had two root canals on back teeth in my late 20’s. Flash forward 30 years and I had three root canals (front area) in less than a year. My dentist also suggested a night guard which I had made and now wear.
I’m supposed to go back in a week to follow up with the endodontist. At this point I don’t have high hopes this 2nd root canal has worked. I just wish someone could tell me what is going on! I’ve had a ton of X-rays along with a 3D scan. I’m so frustrated with this one tooth. Do you think an apicomectomy (spelling?) is next? Then what if that doesn’t work and I have to get an implant? I’ve already spent a lot of money.
Sorry for the dissertation, but I hope you are able to give me a little insight. Thank you.
Good Evening and Happy New year,
My story….I had a root canal approx. 15 years ago on tooth 13. My memory is faulty here, but another root canal was performed on same tooth 5 yrs ago and just 6 wks ago an apico. The apico has failed I believe as the gum at incision line is sore and has developed pus filled pimple. Clindomycin calmed this somewhat but pimple has returned. This tooth is a part of a bridge. Dentist has recommended the tooth be pulled and then have an implant.
I have only had digital xrays and my concern is that i won’t have enough bone to support an implant, as I do have fairly severe bone loss on my upper left-quite significant on tooth behind this one.- I am wondering if I should have a second opinion on how to proceed, and by whom? Endodontist? Periodontist?
And then of course the possible risks to other teeth around this one….. We touched on a 4 tooth bridge but that tooth is wrought with bone loss (in the back). Where to turn? Also, how to seek an expert in my area. I am 61
I just had an apicoectomy in tooth #9 and was not told of the rather large failure rate. I went about a year and a half after the root canal with pain and it turned out to be an infection. I requested to have the tooth pulled but was talked out of it. The infection never showed on the x-ray and was only evident during surgery. Does this mean that I did not suffer bone loss? I am mortified at the idea of getting bone grafts and an implant. Also, my sutures fell out after a few days and I have a hole in my gum, but I don’t see bone through it. I had it checked out and am told it will heal. However, I am wondering if this complication will make it more likely that my procedure will fail. Also, I have experienced horrible sinus problems since the root canal and was told that the two were not related. Is it possible for an infected #9 tooth to cause sinus infections? Thanks so much for any advice.
I had root canal therapy performed on #3 which failed almost immediately (within weeks) so they followed up with an apicoectomy. This all took place around 2002/2003 – I was in my early 20’s. That was after silently harboring this abscessed tooth for almost 10 years (due to being a child who was fearful of dental work). All was well until last April (2018) when the crown suddenly fell off. It was re-attached without event but fast forward a few months to February 2019- and now the notorious gum pimple has arisen. CT performed and sure enough- root fracture. So all-in-all, I am actually really pleased with the ~17 years that I got out of that apico. Sometimes they can last, as was the case with my otherwise troublesome #3. (Side note, #4 never developed, I am lacking 8 permanent teeth, four wisdom teeth and four molars- so I have milk tooth #A sitting mesial to this troublesome #3- which I am very lucky to still have as I approach my 40’s, so if the bone loss is a major issue- I am going to be in trouble without an implant in position #3- yikes!) Good luck!!
Hello, I have had 2 failed root canals on tooth 15 which now has a perforation into the sinus and full sinus. Endodontist then recommended pull the tooth. Oral surgeon said 2 options: pull tooth or apicoectomy. What would you recommend?
if endo says extract then that is the way to go! Endo would have done the apicoectomy if they felt it could be saved
Hello. Within the last year I had tooth 14 treated for a failed root canal – one of the roots in the prior canal was missed, became infected, unknown to me (believe it or not) and caused a fairly large amount of bone loss. Once the apicoectomy was done, the results were analyzed indicating that a cist had been in there for, who knows, years.
How did I get to the dentist? A lesion finally appeared on my gum and pain did happen then.
So after a year, the bone above the tooth is yet to heal – though there has been some healing and improvement. The xray of the area looks like there might be infection again, but I am not feeling pain (I suppose due to no roots in the area to trigger the pain response?).
Do you think the best course is to wait to see if the healing is indeed happening or should I pursue having surgery again to attempt addressing the infection?
Very grateful for any help or questions to clarify what I am dealing with. Thank you so much for having this place to get help as this is such a confusing thing to deal with.
Be well.
Wait it out if you can….re-assess in a few months…hopefully you can keep the tooth!
I had an apicectomy 2 months ago …it was a very ruff surgery . After the initial swelling from the incision went down , I had a larger lump above the tooth , this time with severe pain . No pain before procedure .
Took over a week to get seen , called back for an antibiotic , which they did . Saw md yesterday , said it needed to be extracted . I have read 90% success rate with apicectomy , but I am not in that percentage .
I now have to wait another week to get a second opinion . My advice would be to pull it and save about a thousand !
Hope all goes well for you .
Hello Dr and thank you for this valuable insight.
I am at the point where I have to decide whether to have apicoectomy or implant for tooth #19. My endodontist says my root canal has failed on all roots and the apico has to be performed on all roots which makes success rates lower. I am 34 and had my root canal procedure 4 years ago. Would the implant be more logical for me?
Thank you
In your case with that particular tooth I would say the implant is a better option
I have a crown on tooth #12 where a root canal was done many years ago and an Apico 2 years ago. My new dentist wants to replace the crown because there’s an opening or gap in it that she feels could allow bacteria in (and sometimes food does get stuck). However, I’m afraid that if we tamper with replacing the crown we’re asking for trouble somehow. I would hate to have any further issues or problems and feel I can live with everything the way it is UNTIL the day comes where I really must replace the crown. Is this reasonable, and am I correct in feeling that if we replace the crown now we may be asking for further trouble or complication?
it sounds like what you have is a very common “open margin on a crown.” If I had an open margin in my mouth so would definitely have the crown replaced regardless of the tooth. If you really question that you should see a second opinion provider. Best of luck
I had an apicoectomy 10 days ago. I have a gaping hole and it does not look like there is enough gum to resuture… and I can see bone……….my tooth hurts worse than it did before the root canal. I go back to the Oral Surgeon tomorrow to let him look at what is going on. I am terrified. What has happened with this procedure?
“dehiscence” which means open wound. It will heal. He will repair itself it will just take some time and does not necessarily mean it has failed
I have had an apicoectomy a few years ago and I’ve had a spot on my front tooth. I had previously broken the tooth in an incident falling through a a windscreen of a car and my tooth died. I was 7yrs old and I think they did a root canal. So I had an apicoectomy done I think in 2015. My dentist has told me they will try and see if they can re do the root canal. Or do another apicoectomy. But I told her I’ll end up losing my teeth anyway. She said there is a chance. I did speak to her about getting a dental implant and she said we can look at that after she gets some more advice. What would be the better option? To get it re-done or have a dental implant but the dental implant would depend on my bone structure and I don’t know whether it’s any good. Can you please give me some advice on what would be the better option? I feel that if I get a dental implant, in the long run I save myself the cost of having to get more things done to my teeth especially as it will change my teeth appearance. I’ll have to get treatment to correct them most likely. I love my teeth and I look after them so well. I’m heartbroken. I cried my eyes out at the dentist. Am sat in the car still crying. I’m 27yrs old. This should be happening when I’m much older!
If it is predictable that another apicoectomy may last another decade then at your young age that would be my suggestion. the reason I say this is because dental implants are not permanent. Although they have a very high degree of success when done with a skilled provider and a healthy patient they are not without complications. You really need to be worked up by Implantology Only dentist to really weigh out to the pros and cons. I would not base this on cost although sometimes that seems to be the most important thing. Of course there are many many apicoectomy teeth that I have to remove and replace. I think I did to this week alone!
Dr. Ramsay Amin, hope to receive some advice. Had my first ever root canal of the #9 tooth, Front top left tooth. At age 60 mind you. There was an abscess there,but no pain whatsoever. so a root canal was performed. They completed a filling in the back of the tooth. The abscess has remained. It fills up, and then drains. I have been on 3 rounds of antibiotics. The dentist wants to continue on this treatment. They are also talking about an apicoectomy of the tooth. It’s very stressful, on all sides due to the fact I am on social security disability, and only have a dental health savings plan. This is all very costly for me. If you have the time, I would appreciate your expert advice. Thank you, Mary
hmmm….make sure you see an endodontist for another opinion. If you have implant questions, they are welcome as that is my specialty.
Hi Dr. Amin,
I’m certain you’re a very busy man, but thank you so much for this article it was very informative and shed great clarity. I had two failed root canals, then an Apicoectamy on the same tooth, one of my lower right mollers just over five years ago from a renowned Endodontist. I’m just wondering if it is fair to ask for some kind of discount or something due to the recurring issue. My apologies if you’ve already answered this question. Bravo to you in your great expertise.
You can ask, but it sounds like all “herodontics” have been attempted. No harm in asking especially from a loyal, long-term patient that refers their friends. 😉
Hello Dr. Amin,
I have my 3D scan and would like your opinion on success/failure of apicoectomy and possible solutions. Link to my 3D scan I have a added to Website field. I have RTC done on #16 and #26 back in 2001. #16 has no symptoms with small formation (cyst) on apex. #26 is symptomatic, random swelling and/or flu like symptoms, big formation (cyst) on apex. My endodontist claims it would slim possibility to get RTC revision due to cemented posts, there is a big chance of root breakdown. Would you be so kind to take a look at my 3D scan and give your prognosis on apicoectomy on both #16 and #26? May major concern is #26. I was advised by oral surgeon to proceed with #26 extraction, cyst removal with NO bone grafting. Later in about 6 month proceed with sinus floor lift and just then after another 6 month or so do implantation with possible bone grafting due to bone loss. Would you totally rule out #26 apicoectomy with bone grafting to keep sinus floor? If #26 apicoectomy is not possible why not to bone graft both cyst space and extraction socket to prevent sinus floor landing and alveolar ridge resorption at the time of extractions/cyst removal? I would be thankful for your opinion.
Hi Art, I would love to answer this one question, but I would have to ignore everyone else. I would love to spend 30 minutes evaluating your scan, but I have to see patients, etc. I would be happy to see you as a real patient to be able to give you a diagnosis and treatment plan.
You also need to be evaluated in person as x-rays are only 50% of the story.
Very Respectfully,
Dr. Amin
Dear Dr. Amin,
Thanks for your honest reply. Unfortunately I am not in US, so no chance I could come as a real person. I have so many conflicting information and it seems every side is trying to “sell” their way. Endodontist is claiming root canal re-treatment is my holly grail and it will help to get rid of the 10.4 mm cyst over time, surgeon has the only option to extract without bone grafting, implantologist…
Could you please let me know just in theory is it possible/advisable to extract #26, remove cyst and bone graft at the same time? Bone grafting seems logical way to keep sinus floor and preserve socket for delayed implantation.
Thank you very much in advance.
Yes. This can be done very predictably with high success. 😁
Hello Dr. Amin,
I had one root canal done when I was 17 years old, i 40 years old now and I have recently presented an abscess on the top left tooth next to my front tooth where I had the root canal done with an infection that has started to spread to the bone. At first my dentist had recommended for me to get a apicoectomy, then he said it was a 50% chance that it wouldn’t work due to the Sever infection. He has recommend for me to get my tooth extracted and have an implant. I’m not sure weather I should try the apicoectomy or get my tooth extracted. I have discomfort but no pain. My tooth has discolored and I feel it weak. What do you recommend me to do at this point.
each situation so case dependent. If there is available bone to place an immediate implant with an immediate temporary this may be your best option. Sometimes in the front of the mouth partial extraction/socket shields should be considered for some unique cases where your bone and gum are really thin. Without senior exact x-ray there is no way I can really tell you for sure whether to pull it or to save it..
Hello Dr. Amin
If received a CT scan and there is radiolucency on the scan at the Apex of #7,8,9,10. These teeth had root canals, posts, and crowns 20 years ago but are asymptomatic today The endodontist suggests the result points to infections (active or otherwise).
Are these teeth able to receive immediate implants or does something have to be done with the “inactive” infections anyway at the apex?
I have an endodontist who found 7 teeth with this scan and says i need 4 apicos and 3 need root canal retreatment.
I feel the money would be better spent on implants but the endodontist acts as if his procedures will be 100% successful and that I just had poor dental work done.
The endodontist also says the apicos DO NOT affect my ability to get future implants.??
Should I leave these alone or are these just infections under control that should be removed?
I can’t afford to treat teeth over and over in my life just to later find out they are a source of Chronic infections.
Essentially, before the radiolucency showed at the 4 apexes I didn’t suspect a thing. Can these teeth treated 20 years ago be harboring low level infections? Do bacteria really reside in these root canal teeth microtubules always? Are they always a source of infection or can these teeth really be sterilized??
My current feeling is that root canals are a failed therapeutic option and that all root canals are a source of Chronic inflammation.
It is very possible that you had very average root canal done. Often times retreatment is very successful. There is no doubt that route canals that are not healthy cause a low-grade chronic inflammation and possibly a low-grade infection.
It is going to take some soul-searching and perhaps a few other opinions to decide whether or not you want to extract the teeth and go with implants were retreatment with Root Canals.
Also does not need to be an all or none decision. Perhaps only one tooth needs to be extracted and the other six teeth can be saved.
There is no doubt that some dentists are more skillful than others. This is true in any profession.
I am not opposed to root canals. I would have one done in my own mouth if I needed one .
Hello, I had a root canal done on tooth #11 several months ago. I had a significant amount of pain during the procedure (done in stages). It has been completed a few weeks ago and is still causing me pain. I have been on several rounds of antibiotics already. I am considering pulling the tooth and having an implant. I have inquired and most people do not wish to pull this tooth. What is the success rate of implants in this area? Should I have the tooth retreated?
Retreatment would be the first option that I would do if it were my tooth. Especially if it is only had 1 root canal. You likely have extra nerve canals. I would suggest you see an expert endodontist who specializes in root canals only.
I ended up having an Apicoectomy on this tooth (#11). I got a second opinion and there was infection found at the apex of the tooth and endodontist thought he could not reach it with regular retreatment. There was an extra canal. If this fails, can I still get an implant in this area?
YES!
Just want to say thank you I know it can’t be easy to respond to so many messages but really appreciate your insight into dental implants and giving hope to those of us who have failing root canals and teeth issues!
Hi Dr. Amin,
I had an apicoectomy done 8 months ago on my #9 front tooth. Ever since the initial wound healed, I’ve had a small pimple recurring in the same place around the surgery site that drains on its own. I have seen my endodontist about 4 times asking about this issue, and at every appointment he takes an x-ray and says it is healing fine and there is no infection. He says the gum looks great. We see no lesion. He claims the small pimple is due to granulation tissue at the surgery site. To treat this, he cauterizes the small area of tissue, and the tissue grows back fine in 2 weeks. Once the area grows back fully, it continues to exude small amounts of fluid again. I have no significant pain or swelling and the crown is not loose. I no longer have any tenderness when I press on the area. It is only a small area of tissue that seems to be immature. Should I be worried about this? Or should I just give it more time to heal completely? Have you ever seen successful apicoectomies where the healing process involves a very small recurring pimple due to granulation tissue?
Best, Andy
No —-Have you ever seen successful apicoectomies where the healing process involves a very small recurring pimple due to granulation tissue?
A simple no? Thats all you have to say? You have no other input or questions about my case? What should I do then?
Andy….I am simply trying to reply to you in a timely manner because I care about you. I am a dental implant specialist not an endodontist. This is a dental implant blog forum. My best advice would be for you to see another endodontist (Root canal specialist) to see if the tooth can be saved. If it cannot then you may want to consider a dental implant.
You are not healing normally. You have a fistula.
A dental implant in an area of an apicoectomy tends to be more complicated because of existing bone loss and scar tissue.
Best of luck
My apologies, man. This apicoectomy has been a source of anxiety to me. Perhaps this forum is not the proper resource for my case. May everyone with dental issues be free from suffering and the ROOT of all suffering. Haha!
I really want to laugh but not sure if that was a side note of humor because just the way the question wording “successful apicoectomy ” is sort of an oxymoron in relation to symptoms of the pimple which is infection draining which means the apico didn’t really take care of it
Hi, i have this exact same thing happening to me now. This little pimple above the site. I pop it multiple times a day too. I dont want to have to go back that procedure was traumatizing. If you get any great answers that does not call for a dental implant, or remove the whole thing. Why would i go through all that and 4 months after get the tooth pulled. I hate that we have to go through these teeth issues. I will say it again IHATE TEETH
Because it’s only been 4 months since your surgery, your bone is probably still growing back where the surgeon drilled through the jaw bone to access the root of your tooth. This takes 6-12 months for the bone to regenerate, so it is still too early to tell whether the procedure failed or not. If your surgeon used a grafting material to fill the hole and facilitate bone growth, the little pimple could be due to the grafting material trying to make its way out through the gum. For 6 months after my apicoectomy, I saw little white particles coming through my gum when I had the pimples.
However, you should DEFINITELY call your surgeon and have them look at it and take x rays. They should be able to tell whether the site is infected or if the bone isn’t growing back properly.
Also, try not to poke around the surgery site a lot as this can introduce bacteria. Rinse with alcohol-free mouthwash or saltwater to keep it clean in the meantime.
Andy it’s been 5 weeks since my Apicoectomy, I notice tonight that a pin prick sized hole has white particle there, when I pressed it came out also with watery fluid, I’m scared it’s re infected but could it be still healing?
This has made me so anxious 🙁
oh gosh….does not sound good. Sorry
oh gosh….does not sound good. Sorry.
Also, how bad is smoking long term for the health of a tooth with an apicoectomy?
Thanks
Not great but not terrible. It would be more of an effect during the healing of the apicoectomy rather than after the apicoectomy was done. Smoking causes bone loss around your teeth and turbo charges periodontal disease. Most of my patients that require full mouth extractions are or were smokers for some extended period of time. Smoking also causes implant failure and bone grafts to heal very slowly
Hello Dr. Amin
If you receive a CT scan and radiolucency on the scan points to infections on #7,8,9,10 which had root canals, posts, and crowns 20 years ago but are asymptomatic, are immediate implants an option or does something have to be done with the infections anyway ?
I have an endodontist who found 7 teeth with this scan and says 4 need spics and 3 need root canal pretreatment.
I feel the money would be better spent on implants but the endodontist acts as if his procedures will be 100% successful and that I just had poor dental work done.
Hi Dr Amin. I had done apicoectomy on my #11 two weeks ago because i felt a bump in my lower nostril and my dentist recommend me to have a xray and saw an abscess and need to do apicoectomy. After 1 week of apicoectomy felt a bump again in my nostril a little bit upper than before. And I felt discomfort on my tooth. Is this the sign of unsucessful surgery? What will I do my denstist says its for observation. But Im very worried about it because I thought after this everything will be okay.
Unfortunately this procedure is not always successful and is considered a end-stage treatment for a tooth. I hope it works out for you. Fingers crossed!
I have been told I need to have a tooth extracted #19 that had a root canal and crown about 14-15 years ago. I want to save the tooth, and was told an Apicoectomy could be done but has a low chance of success. I have been referred to an endo for a consult, my question is should I try and save the tooth what are the odds I can save it , will I have a problem with trying to get an implant in that location because of the root canal ? As I recall I went to a root canal specialist when I had the root canal done because it was a curved root.
hmm…each case is pretty unique. I do some apicoectomy is BUT….only when I am certain that it is going to have a high degree of success and the tooth will stay for a long time. You should have the conversation with your endodontist about longevity and expectations so you know what you are getting into. You will likely still be able to have an implant after having an apicoectomy if that fails as well.
Hi, i am also having issue after a apicoectomy. It was done early decemeber. Two weeks ago i felt a bump on my gum at the site he cut open. There was pus so i popped it, i have been using an oral antiseptic after everytime i pop it. I hate the dentist hate hate hate. I have been traumatized since the last procedure and do not want to see the endo dr again. Why do i have this now? Will i have to be re cut open? Help cause i dont wanna do this again! Thx
If it does not work you will basically need to extract the tooth. You should consider being sedated for dental work so that it is more pleasant. Many apicoectomy procedures are not successful… but a few are.
Hello Doc. Amin,
Few days back, I visited my dentist for a cleaning where they noticed a swelling and a bump above tooth #10, after taking an x-ray there is a definite abscess showing above tooth #10,and #9 , both previously treated with RCT few years back.
My dentist referred me to the endodontic, and he suggested the epicoectomy, and before I decide to do this or have teeth extracted and place an implant , I would appreciate your opinion so much.
At this point, one of the teeth has a post, so he would not be able to do a regular RCT procedure on this one. However, the other tooth could and he suggested to preform epicoectomy on both at the same time.
Now, I am just so desperate in making the best option either finishing the procedure or extractions followed by an implant. The endodontist said I don’t have any concerning high pockets, or any gum retention issues. I am hoping you could share your thoughts, I would greatly appreciate it.
Thank you,
Take a 3D scan BEFORE doing anything. Be assessed by an expert in implant dentistry see if you wouldn’t even be a good candidate for implant or not. Some implants are far more complex than others. Some people also have genetically her really good bone shape and thickness while others have terribly thin bone that is prone to complications.
I am scheduled to have apico surgery in January on #12 and #13. My issue is all symptoms, swelling and pain, have been gone since Thanksgiving when I took an antibiotic. I’m wondering if I even need the surgery anymore. My dentist says yes. Endodontist hasn’t responded. What are the risks if I cancel?
Most infections around root canal teeth wax and wane. Meaning they have good days and bad days. See with the endodontist says and then take it from there. The longer you wait the less chance of long-term success.
Hello,
I had my first root canal on #3 a few months back and an apico on that tooth 4 days ago. This was set into motion a year ago when I had mild sensitivity during allergy season. My dentist corrected my bite, which threw off my entire mouth and caused the start of TMJ. He eventually put a crown on that tooth and I had a specialist do DTR treatment for the bite and TMJ.
However that tooth remained extremely sensitive to cold and eventually started to erupt causing more bite issues. I found who I hope is supposed to be a very good endo who diagnosed me with irreversible pulpitis and did the root canal that day. He did a CBCT before hand and used laser treatment in addition to standard root canal treatment. I had the crown filled and bite adjusted and the tooth was awesome for about a month or so. Then the bite started to become high again and I had mild sharp pains when biting. No matter how many times the bite was adjusted it always became high again a few days later! I went back to the endo and he repeated the CBCT and found that while the root canal itself was excellent, two of the root tips were not. He said an apicoectomy would take care of things for me. So that’s what we did. He used laser for the apicoectomy, said it was more precise and less pain and damage that scalpel and burr.
So I’m now on day 4 or 5 post treatment and while I have some sinus irritation on that side, there’s not really a whole lot of pain. I’m only taking an Advil here and there along with a course of penicillin and occasionally a bit of pain meds at night, mostly to help me sleep. My question though, the bite on that side of my mouth still feels a bit off. I know that tooth has had what is basically trauma done to it and with the swelling I’m not surprised that it’s off. So is this normal and should the bite return to normal as it heals? Or should I go have it adjusted? If so, how soon? Should it just be fixed as normal or taken out of occlusion all together? It doesn’t feel like it’s moving or anything, just feels strange, and there is some TMJ irritation on that side (mild joint and ear pain and muscle spasm). I do have a bite check/DTR follow up mid June. Should I move this sooner? My worry is if we take too much off then it will cause problems for the surrounding teeth and then I will have to get the crown replaced again to fix things.
Thank you
Danielle
My speciality is implant dentistry but I do some apicoectomies when I am certain they will work. You want want to visit a root canal forum.
Hi Dr. I had a failed apicoectomy 11 mos ago on tooth # 10 followed by extraction of the tooth and bone graft 7 mos ago. I have intermittant congestion in the left nostril. At night, left nostril is clogged if I lay on my left side. If I change positions and sleep w/my right ear down, that nostril fills. When I get up, the nostrils clear but it feels like post nasal drip down throat. During the day I have some sensation of left nostril getting when I eat. The oral surgeon took a 3D scan and says he sees no problem related to the tooth. I am due to have the implant placed next week. I’d like to have a front tooth again but am worried that nose issue is tooth related and may get worse when the implant is placed. What would you advise?
Hi Dr. I had a failed apicoectomy 11 mos ago on tooth # 10 followed by extraction of the tooth and bone graft 7 mos ago. I have intermittant congestion in the left nostril. At night, left nostril is clogged if I lay on my left side. If I change positions and sleep w/my right ear down, that nostril fills. When I get up, the nostrils clear but it feels like post nasal drip down throat. During the day I have some sensation of left nostril getting full/congested when I eat. The oral surgeon took a 3D scan and says he sees no problem related to the tooth. I am due to have the implant placed next week. I’d like to have a front tooth again but am worried that nose issue is tooth related and may get worse when the implant is placed. What would you advise?
The two are likely not related. Many patients have issues with their sinuses. Others have nasal passage issues. Some have both. I would suggest you see an ENT and scope your nose BEFORE you have the implant.
I don’t think it is a related but I do think you should see an ENT physician and have your nose scoped prior to having the dental implant procedure. This will give you peace of mind and a better expert opinion in that area of the face.
Hi, this is day 2 post my apicoectomy on tooth #10 and I feel like the space between my nose and upper lip has increased as if my upper lip has been pulled down.. is that normal during the process of healing? I’ll have my 3 stitches removed after a week. I’m worried that these changes will be permanent!
Not permanent. It will resolve soon. 🙂
Hello Dr. Amin:
First I would like to thank you for creating this site. It has been very informative and on some level, comforting, to know there are many individuals who share in dental woes like myself.
I had an apicoectomy about six weeks ago simultaneously on #5 & #6 and have a few questions:
Tooth #6 had RCT many years ago and the post broke off after biting in to something too hard. My dentist did another RC, and discovered # 5 had issues of its own (that tooth also has root canal/crown). About a month later I developed a pimple above #5, and was referred at that point to the Endo who performed the procedure. My stitches healed nicely, however #6 feels a little loose, almost like there is a little give when I bite down. I have no pain or swelling. Do you think my procedure has failed? What are my options going forward? Any insight you can provide is most appreciated.
bite adjust it ASAP and have them look for something called “fremitus.” That is going to be the best chance that you will be able to keep this tooth. It is basically moving when you bite which is the kiss of death over time
Hi Dr Ramsey:
Update on my apico. Both teeth are a success! Everything healed nicely after bite adjustment. Thank you again.
😁😁😁
A couple years ago after a failed root canal on tooth #7 I was sent to an endodontist because they couldn’t find all the canals during the first treatment. After the retreatment I had pain again after several months and had an apicoectomy on tooth #7. Afterwards I had no pain. In the subsequent check ups: one being a week later to remove the gum stitches and the second being a 6-month follow up I still had no pain and the specialist saw in the x-ray that the bone had healed and infection was gone. Now about a year removed from the apicoectomy I’m feeling a slight dull pain or discomfort and can come and go and never lasts long. The tooth is not hot or cold sensitive or sensitive to the touch, although it has a crown. It feels deeper than the tooth so it may be the bone.
Hi, I had an Apico on my top #8 tooth it’s been about 3 years, sometimes I notice some soreness, but no gum pimple or redness. Is this normal? Is the only sign that an apico has failed extreme pain and or gum pimple. Is it worth looking into?
Definitely worse looking into. Usually a gum pimple is the main sign of failure. A 3-D scan would be very beneficial.
Just recently I’ve been told/diagnosed with severe bone loss between tooth #8 and #9, unfortunately bone loss goes into nasal cavity/wall. I’ve had two root canals on tooth #8, last one completed around 2015, saw a pimple/abscess just above the gum area, became extremely painful, so went in to see dentist. He referred me to an endodontist which gave me the bad news. Endodontics suggested that I see ENT for full evaluation and recommendation. I’ve been on antibiotics for 3 weeks, 2000 mg of Amoxicillan a day to control infection. Maxillary specialist at ENT recommended tooth extraction, bone graft, with future prosthesis or implant with an oral surgeon. I’ve had two oral surgeons who state my case is complicated and not willing to take my case. I don’t know if I’m understanding my prognosis and if it is worse than what I understand.
Come see me if you are local! I treat the toughest cases 😉
Hello Dr.Ramsey.
I wanted to ask a question which is mocking my mind. I has an apicoeotomy surgery on one of my upper teeth. One month after the surgery(now) I started feeling a slight pain in the area near my left nostril. Also, my gum is swollen ,but without pain in it ,however, the tooth which had the apricoectomy surger done to it and tye tooth beside it are hurting meand the pain is unbearable when I bite or even touch the tooth itself. I am very confused. Is that a normal thingor is it not? It is just my bone hole is healing after the surgery and thats why its causing two teeth to hurt?
This procedure is very deep inside of the bone. I always make sure that my patients have an intravenous steroid just before the procedure begins. Without it, it is a long painful recovery. I suspect it will take some time before it gets better. Sorry.
Hello. I’m a 58 y/o RN. I’ve had 10 root canals and 15 crowns in my life. All went well until last Sept. I told my dentist I felt that something was wrong with tooth #3. He said it’s probably sinus (I don’t go there anymore). In Oct, my Endo had retired so I went to another one in the area. It was sensitive to cold and problems with chewing. It was Pulpitis (that’s what I’ve had in all my bad teeth) He started a root canal and had to stop d/t one canal bleeding and inflammation. It was very rough and I wasn’t numb enough. He did not see any infection thus far. He put medicine in and I went back in 3 weeks. He did the root canal and I had horrible pain after that. I knew something wasn’t right. I could also feel a sensation up high on the gum line above the tooth when I touched it. I went back and he said it could be cracked but he wanted to re-do the medicine and root canal again. I went to an oral surgeon who had the cone beam CT and it showed overfill. The Endo called me and said he wanted to change the treatment plan and do an Apico under IV sedation. I wasn’t happy with that so I went to an Endo (who does 2-3 Apico’s a week) for second opinion. He didn’t notice a crack but said it would be a 50/50 shot and I didn’t need IV sedation. I had that done 3 weeks ago (5 months after all this started), and I did fine. He had to do Apico on 2 roots and re-fill the other 2 that the first Endo did. He did not see a crack. Two weeks out, I went to chew on it and had horrible pain. I still feel the sensation above the tooth when I touch it with my finger. I also have off and on pain like I did prior to the Apico. I went back to the Endo and he called in Amoxocillin and it made me sick. I went to my dentist and he said “enough is enough” and we would try a different antibiotic and if not better in a week, the oral surgeon would extract the tooth. He spoke to the Endo on the phone and they can’t figure it out. I’m taking Zithromax and it’s not working either. That’s not what he preferred but all I can handle stomach wise. So, in my mind….I think I’m doing the right thing by getting it extracted and getting a bridge. I just hope too much damage hasn’t been done. I feel that I may have a crack. I just wonder if it was caused by the overfill or cracked from the beginning. Then again, it may just be my tooth. On that note, I’ll never have another Apico. I’m sure I’ll need more root canals. What are your thoughts on all of this? It’s a mess.
Sorry for all of your trouble. When a tooth is that questionable a better option is extraction even if that means a small or large sinus graft for the upper right molar #3. The best endodontist and the world cannot always capture all of the thousands of micro-canals at the end of the root. Also the tooth is very compromised structurally and you may end up having all that done for nothing.
A dental implant for an upper molar is very simple to do and predictable. You might need an internal sinus lift to make it solid but it will be a great tooth for a very long time if done with great skill.
I had two root canals done 3 years ago on the right side (upper and directly under on bottom) towards the molars. The bottom root canal was successful on the first attempt. The top never felt right from the bite to there always feeling like food was getting up underneath the tooth. I voiced this and went back in to see a different dentist at the same office. The dentist who originally did mine was let go and so I was seen by another dentist who examined the work previously done. He expressed his concerns on the root canal not being done properly and he re did the work at no extra cost and very apologetic. There was in fact like I stated an opening from the crown not fitting properly causing food to be able to get underneath and cause gum irritation. After the new dentist re did the root canal the bite still felt funny and they could never get it adjusted to feel completely comfortable, so I dealt with it seeing it didn’t seem as bad. The tooth was half way shaved down than a normal tooth. I started experiencing major discomfort and irritation last Wednesday and scheduled an appointment immediately to find out through new x-rays there was an infection under the tooth, yet they said the newer porcelain crown looked beautiful. The dentist that looked at my new x-rays said she could barley see a tiny canal in those x-rays that was not filled/closed off. I have already spent over 2,000 on one root canal and now I will be sent to an Endodontist to spend another 1,540 to get this canal filled. My question is should that tiny canal have been filled during the initial root canal on the first and even second attempt? I appreciate your feedback and just would like another opinion seeing I am a young college student trying to keep up with bills in general as it is. I would just hate to sit out of school for a semester to get this “emergency” tooth work done as they say to prevent future maybe even larger issues.
Thank you for any feedback or advice! 🙂
Root canals are very difficult and are definitely not 100% successful even with a very skilled provider. There are thousands of miniature nerves at the end of the root that cannot be filled. Ask the endodontist the prognosis on this tooth before doing anything. If it was a really terribly infected tooth to begin with long-term overall prognosis with a root canal overtime is not great.
Had a root canal about 3 years ago maybe a year ago and I never got it capped and I was trying to get something out of my gums and my tooth came out what does that mean
if root canal has high chance of failure why not do apicoectomy directly?
That would be way too aggressive when a root canal works most of the time. That would be like cutting off your toe instead of fixing an ingrown toenail. If this is the second time you’re having a root canal done than a simultaneous apicoectomy can be beneficial
Hi, I posted a question a while ago; could it be in your spams? Thanks!
please repost if it is a unique question that has not been previously answered.
I had an apocectomy done 25 days ago #14, but I have pain around my eye, as well as cold feeling on the left side of my head and my arm. I took antibiotics the first week and the pain on my eye had dessapear, but now is back, and I am taking more antibiotics prescribe by the Endodontist, but antibiotics are not helping, do you recommend waiting, or should I get the tooth pull out?
CT scan was taken before apocectomy and they said that the chance of success was very high, but With this pain and discomfort in my eye I am panicking now. Please help!
Watch this video on antibiotics. I would suggest that the antibiotic family is switched altogether.
hello, i found this post thru google.
my dentist told me i would need my two upper front teeth, extracted, since there was not enough bone in the upper jaw, under nose, area for an implant.
i don’t really know that this is a good idea, although i am not a medical person whatsoever.
i have a deep overbite.
i really wanted an implant, but he stated not enough bone.
is there another option to have normal teeth appearance, without a partial?
thank you
Sometimes in the upper front part of the mouth a dental implant is not a good idea if you have a very thin bone structure. Sometimes even bone block grafting will not correct this because of genetics. I would suggest you see a second opinion of a very skilled and experienced implant dentist before committing yourself to inferior treatment.
YES I HAD MY ROOT CANAL REDONE 3 YEARS AGO. I HAVE THIS RED BLISTER LIKE BUMP ON MY UPPER GUM WHERE I HAD MY ROOT CANAL DONE ITS BEEN 6 MONTHS AND THE BLISTER RED BUMP STILL THERE. WHY HASN’T IT GONE AWAY?
The problem may still exist or it could be scar tissue. You need to have this checked out.
Hi . I had apicoectomie almost 1year and half ago. But doctor said no need for bone craft the will recover by itself. Now I feel like a pressure in the area and pulsating sensation… What it could be . I have feeling it is not normal.
you will need to take a CBCT 3-D scan to really evaluate the area. Apicoectomy teeth are difficult to evaluate by traditional x-ray.
hello! I am 22 years old and i have 6 tooth missing since i was younger and have not gotten them replaced..two tooth at the top left and 4 on the back bottom of the left and right side of my mouth. My question is one of my top left tooth that is missing, the gap has closed I’m guessing because my teeth started shifting since i waited so long to get dental implants, what are my options for that gap that is now closing? will it affect my other teeth later in the years being that i can’t replace it with a dental implant?
You can do orthodontic correction and upright the teeth that are tilted to make proper spaces for dental implants. This will restore your bite back to normal which is the right way to do things.
My dentist performed endo in 2013 on #13 (with an onlay) and it took a year to settle down. Unfortunately the pain (infection) return and in November 2015 the endo was redone by a specialist It has been a year of off an on pain/pressure, usually originating from upper cheek. I had xrays and a CT scan at the hospital, all showing no sign of an infection and the specialist said it looks fine and give it time. Isn’t the CT scan same as 3D? I’m not sure what to do, I don’t want to pull it if there is no sign of an issue but can’t live with the pain. .
it is likely fractured vertically and it will not show up on the scan. That is the most likely scenario which will lead to down the past unfortunately of losing the tooth. Sorry for the bad news. A 3-D scan is the same as a dental CT we call a CBCT.
Thank you Doctor. I have no biting pain or temperature sensitivity, could it still be a fracture? The pain/pressure commences is in the cheek area but eventually leads to tooth discomfort. I eat/drink without any pain, often times eating/drinking relieves the discomfort, that’s the strange part.
Yes, fractures have symptoms just like you describe
thanks for give a such guidance about what are the benefits are included in dental treatment. keep sharing more on dental treatment.
I notice a small white spot next to the end of the root in one of the pictures. My dentist, upon taking a panoramic x ray, found a small, well defined white spot next to (as in to the side of) the end of the root of a tooth on which I had a root canal and crown earlier this year. It’s slightly larger than the one in the picture in your article. They said they hadn’t seen such a thing before. I’m speculating that some of the filler escaped into an abscess (which is what prompted me to get the root canal in the first place). Any other ideas?
That is likely the case.
Tooth # 6 had serious pain and I underwent a root canal. 6 months later, severe pain again and I had an Apicoectomy. Pain went away for 7 months and now I am in severe pain again. Saw my regular DDS today and he X-rayed the tooth. On X-ray he did not see any retrofill at the top of the root. Does retrofill break off or disappear? I know the tooth is not fractured, because the pain went away after the Apico. Can you comment?
retrofills are not always needed or suggested…often, sealing the gutta purcha and a graft is better than any material!
Mydentist just closed down&told nobody so i dont have access to dental records but,on the topfront i have 4crowns the 2nd left one has had root canal& apicoectomy as far as im aware ,now i have an absess an im not sure whats the next option for me or the best way forward,im in some pain an feel it effecting the other teeth,please advise me …
Having a burning feeling 4 weeks after apesectomy .
Is this normal , does this mean tooth and bone is mending .tooth next to it feels sore when this happens .
Dentist can’t see a problem yet .
I am getting anxiety about this situation . Felt no discomfort after operation . Gum has healed perfectly .
Please help
“The worst case scenario is where the “apico” fails and the entire outer bone wall is lost.” What are the side effects of loosing the outer bone wall?
It is critical!! Without that bone you will almost certainly need a graft to build it back. That bone is usually less than 1mm thick in the upper jaw and front teeth in general. Some people have thicker bone in the back but not usually.
Hello My name is Cynthia and on March 28, 2016 I had my second root canal procedure tooth #15. I did not think anything would go wrong. The Endodontice dentist did not give me any kind of antibiotics when I left. Five days later I went to my dentist and he filed the tooth. Everything seem fine. The seven days ago my tooth stated to hurt again. I have been taking tylenol . It got worst and stated to really hurt. I went to my dentist and he told me I think the tooth is cracked and fractured you have to go back to the people who did this and show it to them. Next day I went to the Endodontics dentist and she said when you left here the tooth was fine. How did this happen. I told her I do not know and I am on antibiotics from my dentist. She told me there is nothing she could do. She did take an xray and it showed a fractured root canal. I am very upset . She told me the tooth has to be extracted and she does not do this. Now I have to go to another specialist to take the tooth out. I am very upset since I do not have money to keep spending on this problem. What do you suggest I do. Please let me know. Should I have had an implant instead of the second root canal. Please give me your advice. Thank you Cynthia
This is a sad story for sure. Teeth can crack immediately after the root canal but before the crown. This is not your dentist fault or your fault. It just happens on occasion. Perhaps the tooth was too weak to save in the first place.
Over the last several months, I have had mild tenderness over the “MB” aspect of tooth #14. This discomfort has become more pronounced in the last few weeks along with some intermittent tingling in my left cheek. This #14 “MB root” has ALREADY undergone RCT (x’s2) and an apicoectomy (2 years ago). Last week my primary DDS did an X-ray which demonstrated a radiolucency/infection at the MB apex of #14. I will see the oral surgeon who performed the “apico” in a couple days for an evaluation. My question is whether I have any options for this #14 tooth short of an extraction-i.e. “amputation” of the #14 MB root or a repeat apicoectomy?
Thank you for your time and expertise!
Unfortunately too much work has been done to this tooth too many times. You would be far better off replacing it in most situations unless you have an extremely long root. Rarely a root amputation can be done in conjunction with a bone graft to save the tooth but again these are all salvage procedures that will eventually end up getting extracted.
Thank you, Dr. Amin, for your input. I proceeded with a REPEAT apicoectomy on the MB root of this #14 tooth. I will keep you posted on the status of this tooth as I move forward.
I am 52 and lost my 3 front teeth when I was 11 after being knocked down by a car. Age 18 I had a bridge fitted. In 2014 after many years of know problems I had a Apicetomy above right upper 2, in February 2016 I had the precidure again, but this time it was worse destroying my bone and tissue under my nose. 10 weeks has now passed and i have an infection in my gum above my right upper 2 and a small hole showing bone. I am on a course of Antibiotics and I am being referred back to the hospital for a follow up. I was just wondering if you could advise me on how they may treat this, and how they will fill this hole. The Doctor at the time said he had removed the infection and hoped the implant would be good for another 3/4 years. Hope you can advise me.
Many Thanks
This is a difficult situation to give you advice via the web. I would suggest you have a 3-D scan prior to any root procedure and definitely prior to considering dental implants
Also you should get into the hands of a very advanced and experienced dentist who can handle complex situations
Had a RCT post and core with crown on tooth number 14. just 3 months after all that got a little bony bump on mb root. Big radiolucent area. No pain for a year then got crazy flu and it started to bother, so got an apical done and after 3 weeks right when finished antibiotics got the bump back now it is bigger then before, again no pain. any suggestions ?
It sounds like this tooth has had a ton of work. Eventually it will likely be lost that hopefully you can hang onto it for a bit longer long as the radiolucency and infection clears.
May I ask. 2 years ago I haf RTC but it failed the doc. said need to took an epicoectomy. In 2 years I was been feeling something weird on the tooth who had an epicoectomy sugery. It.don’t have pain but when you touch it something on pressure. I took an xray from dentist . She said there’s on the canal that looks like not clean. She told me the risk bec. I.my root is very weak she said rather to take off the on my upper from #22 . If the retreatment root canal not successful on are of epicoectomy. Is that true ?
I don’t really understand your question. Can you please re-word?
Went to the endodontist last February 2015 had root canal done on tooth number 30. Post and crown where done. One year later I’m experiencing severe hot sensitivity.. I’m going back to the endodontist that originally did the root canal…had new X-rays done (not 3D)..my question is: if they have to reassess the canals do I have to pay for that procedure? I’m on Medicaid and the insurance covers nothing!!!
There is a good chance it is a different tooth if you’re feeling temperature sensitivity
My father is 70 years of age and has a root canal on tooth #10 that was done many, many years ago. Upon his first dental here in the USA last week, the dentist detected a small stain on this tooth as a possible infection (we don’t know how long it has been there but no symptoms so far). My father immediately went back to his dentist in Mexico who cautioned him about the procedure as he rather have my father check on it every couple of months via x-rays to see if the infection grows and if it does, he recommends for the teeth to be removed and have an implant instead. Besides my father’s age my concern is his heart condition and the fact that he is on blood thinners which requires release from the cardiologist everytime there is a surgery. What are your thougths for wait and see on infections that seem to be encapsulated?
I would take a 3-D scan prior to making any decision. If you decide to wait, just repeat x-rays yearly to see if the lesion gets larger or fracture other teeth. Dental implants are not always the answer!!!
Hear some information about blood thinners
I had two failed root canals in my front tooth and then an apoectomy, 6 weeks ago. I don’t have pain, but the pressure both in my tooth, sinus and my nose is ridiculous. Also the tooth under the crown has gone black…..the surgeon said there was a lot of infection in the bone and had to drill out quite a large hole….he’s saying the pressure is only from the bone knitting together…..but the pressure now is worse than it was when I had the infection….should I just get the tooth out…..is this possible after only 6 weeks of having the procedure.
take a 3-D scan to assess the area
Hello,
I had a root canal and crown done almost 5 years ago, March 4, 2011. A few days ago the tooth starting throbbing and is sensitive when I tap it on the top of tooth, it is #30, back lower right. My dentist gave me amoxiclian and took X-ray and said looked like small infection below root canal and may need a “pretreatment”.
My question is would it be possible for the amoxiclling take away the problem thereby I won’t have to go back to Endotonist for another root canal? The pain and throbbing is much better with the medicine, just periodic slight throbbing and definitely when tap top of tooth sensitive, but can eat and chew without pain.
I am just trying to figure out if I am being talked into an unnecessary and costly procedure or if delaying this will get me sick. Please help, I really don’t know what to do and am on a limited budget.
Thank you,
Lori
there is a very good chance that tooth is fractured and retreatment root canal may not be successful which would end up as a dental implant. Antibiotics do not cure these types of infections. Learn more about antibiotics on this post
sorry for the bad news but I don’t want to see you have another root canal done on a tooth that is about to break. Asked the endodontist if they see a fracture in the tooth. Good luck
I had an apicoectomy two weeks ago but the oral surgeon didn’t ask me to return for a follow up. How do I know that the procedure is healing correctly? Almost all dental procedure requires follow up visits to check if everything is OK
I would suggest you have a follow up soon and then again in about 6 months. At the six month follow up an X-ray should be taken to see how the bone is healing.
I found your page while doing a search- this situation applies to me. Tooth 9, upper front tooth, had a root canal done on it and was crowned years ago after an accident. A bubble formed on the gum on top of the tooth, and even though an infection was not visible on an x-ray, my dentist referred me to an oral surgeon who did an apicoectomy (done about 1.5 years ago). Now I have noticed recently that there is a large, hard bump on the gum above the tooth and feels like it has spread to the tops of the surrounding two teeth as well, I am afraid the infection not only came back, but is spreading. In your opinion, would removing the tooth and putting a dental implant in be the best way to try and resolve this problem?
don’t jump to that conclusion too quickly. Have a 3-D scan taken and evaluate your existing teeth before sending the tooth has to be extracted. 3-D CBCT scans that are interpreted correctly will help you diagnose and give you a peace of mind that you’re doing the right thing. Taking out a front tooth is to be taken very seriously.
I had an abcess drained a few weeks ago. The Oral surgeon suggested an extraction. I went to a second oral surgeon and suggested and apicoectomy to save the tooth and I had it immediately. I have been told that the best suggestion was an extraction since apicoectomy on a molar that already had a root canal was not the right procedure since I might have another infection in a near future.
A couple of years ago, I had a root canal done on tooth 15. About a year later, the toothaches returned and would leave for about 6 months after a round of antibiotics. I did this for a couple of years and then had the tooth looked at by a couple of endodontists. They said the original root canal was solid, but that the infection was not taken care of from the root canal. A apicoectomy or extraction was recommended. I went with the apicoectomy and have not had a toothache yet (it’s only been about 3 months). What worries me though is that the small bubble that was always there, but would fill with puss during the toothaches (before the apico), has not gone away. It’s a little tiny bubble on the gum and the endodontist said it may not be infection anymore, maybe just a spot that has not fully healed up. Is this possible? I am somewhat worried about the infection lingering and causing bone loss in my gums. If it is infection, will it at least manifest with a toothache at some point so I know what’s going on? Is there any way to know what the little bubble is if it is not causing any pain?
Take another 3D scan six months after the procedure to eval the sucess of the apico….that is what I would do.
🙂
I had Apicoectomy done a year ago, but the infection came back. Now my dentist says i need an implant. He says the longer i wait the more bone grafting i will need. Is that correct?
I don’t have enough information to answer this. You really need a 3-D scan and an excellent diagnosis and treatment plan. I’m 95% certain you will need some type of bone graft. What type and technique is the biggest question.
I never had an infection, just off and on a lingering ache in tooth 4.
My dentist did a root canal, however, the lingering ache remained. This has been going on for four years. I just had the tooth scanned and evaluated by an endodontist; again no infections.
He recommended another root canal and evaluate the tooth microscopically. Would this compromise the tooth even more? Do two root canals affect an implant at a later time? Again the tooth has never had an abscess or an infection. Thank you for your response.
A 3-D scan is an excellent tool at diagnosing problems within the root canal system of the tooth. The problem is even though you may be able to see the problem, the nerve may not be able to be filled with a root canal. Some nerve endings branch off into areas that root canal instruments can never reach. If the endodontist feels like retreatment has a good long-term prognosis then by all means I would save my own tooth before extracting it and having a dental implant. Many root canals are unfortunately done very poorly and an excellent root canal can definitely solve the problem.
Best of luck,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology
The only reason he wants to do a root canal, is for diagnostic purposes, to evaluate the root microscopically. Could an apicoectomy be a solution ?
I just think the discomfort is deriving from the apex area. Ever since I have been wearing a niteguard, the pain is much less, but still there. No pain at night and no pain chewing. It feels like a very slight inflamation in one corner of tooth number 4.
Thank you in advance for your response,
Marieke
The scan MUST be done first.
He did another scan and it did not show anything
Sounds like the root has a tiny hairline crack in it. It may be years before anybody can see it. Most cracks are not visible on 3-D scan because they are extremely tiny. Good luck
Dr. Amin,
I went to my dentist with sudden pain at the back of tooth 11 at the gumline after 10 days of watching to see if I had scraped the gum on a tortilla chip and staying off the tooth and gargling with salt water the pain remained. She took an xray which showed a large dark area and told me I had a “resorptive” tooth and would need root canal. I said the part that hurts was at the gumline. She said I had a subgingival lesion and I would need a root canal. She referrred me to an endodotist not on my insurance and I asked to see one that was on my plan. She insisted I at least get a consult. I went to him and he said he would do a root canal and a gum flap (to clean out the bone). No mention was made of a crown and I was told it would NOT be crowned because the materials he would use to fill and seal would make the tooth hard enough..Per this endo the diagnosis is External Cervical Resorption.. I then sought other opinions because of the fees involved and the issue about the crown.. The endo on my plan with a very good rep said, the root canal might never get rid of the “sensitivity/irritation” I felt at the gumline and I might want to consider putting the money toward an implant.instead. He said he did not do the type of thing the other endo does, doesn’t use the same materials and would not take my case. I sought out a periodontist to see f I had enough bone to get an implant and he took a 3D cone beam xray and said – I was a candidate. He told me that the amount of resorption on the xray and th3 3 D CT scan, made the choice of root canal and gum flap a poor choice. The endo he brought in said it was a 2 year fix and I would be back to get the tooth pulled. and said the restoration would be the hard part because of the “margins”. He was shocked that there was no plan to crown the tooth.
After reading your site and knowing how difficult tooth 11 can be to implant (I’m 63 and have osteopenia), and because of the infection affecting the bone in this tooth, I don’t know which option is really best. One oral surgeon told me he would not graft the socket if there was infection present and would proceed with the implant without a graft when socket healed. I would NOT want to jeapordize my chance of success without a bone graft. I hate the idea of pulling my natural tooth which looks quite good but doing the root canal and flap can affect the implant success as well making the extraction more difficult and with gum/bone loss from the flap. I don’t really know what the best option is. Plus when I have asked about implanting tooth 11, so far, I was told it was just like any other tooth and I know from what you said that is NOT the case. I’m happy to email you the xray. And will try from the library where someone savvier about copying and pasting can help. Will the left side of my face lose it’s shape as someone with compromised canine previously said?
best regards,
Fran
sorry for the delay…your post went to the spam filter…I hope you have treated the area…it sounds like saving this tooth would be a waste of money because the root is dissolving. I see plenty of patients much older than you replace their teeth with a graft and implant routinely. The graft of the socket is going to be CRITICAL to the outcome of this implant.
good luck…RA
Had a root canal , post and temp.crown. 3 weeks, no problems. Then I got the permanent crown and 4 days later the crown felt sore. Gums are not sore , Dentist put me on antibiotics with no improvement. Hurting is also up into my face, The crown still feels very sore and hurts.
I thought root canal pins were forever … I had an impression for invisalign it was tough coming off very tough..week later root canal pin broke off. Now left with getting implant
I had a root canal done in 1992 and a retreatment in 2008. In December of 2014 I had an an abscess where my retreatment was done and had an apicoectomy done. Here it is 8 months later the area above my tooth felt swollen and tender. I went two weeks ago to see him and he took an X-ray and said everything looked good and it was probably scar tissue. Here it is now tender and I had white lies come out today. My si us area is tender as well. What should I do? Get a second opinion
Yes…and get a high resolution 3D scan with the best endodontist in your town.
If you can save it, then great.
It sounds like this tooth has been through a lot though….this may be the end.
Sorry!
Dr. Amin.
I had a root canal last year on my #9 tooth due to a small cavity that developed during my pregnancy with my son. The dentist worked me into the schedule that day and said he could do that root canal right then. I have never even had a cavity before and I wasn’t completely aware of what exactly a root canal was but I figured he knew what was best for my tooth. He worked between me and 2 other patients and really didn’t do the best job at cleaning my tooth out. I told him a month after my tooth was still hurting. The tooth wasn’t hurting before I even had this procedure. He said all looked fine. Well 2 months later a pimple developed about the tooth and I was still having a lot of pain and pressure. So I went back again and he said there was nothing he could do and sent me to a oral surgeon for a apicoectomy. The oral surgeon said I had a 80% chance of success with the procedure and he said it wasn’t fractured or anything when he looked inside the tooth. Also I never had a crown put on the tooth after my root canal which I wasn’t aware I needed. 2 months after the apicoectomy the pimple yet again returned and I was in pain. The oral surgeon went back in and cleaned out the infection yet again and I was told if it failed again the tooth would need to be extracted. Well here it is 4 months after the 3rd procedure and my tooth is infected and I’m in a lot more pain. I went to a new dentist last week for a second opinion. She said she could do another root canal through the back of my tooth and save it. I do not have Medicaid any longer and I would have to pay out of pocket. I am only 22 and am a single mother who is only going to college right now. I don’t have the money to pay for a 4th procedure. She mentioned a payment plan so I’m trying to determine if it is worth doing another root canal after 1 root canal and 2 apicoectomys already? If I get my tooth extracted all I can afford is a flipper tooth which she said would not look right do to how my front teeth are shaped. But something has to happen because I’m starting to get bad headaches and I’m very nauseated from this infection. I have taken several rounds of antibiotics. What would your opinion be? Any advice is greatly appreciated and I thank you for your time.
Take a 3d scan of the tooth to evaluate the quality of the apicoectomy, root canal and possible fracture of the root.
Find the very best endodontist in your city and go see him or her. That is what I would do. Try to save your tooth if it is possible but it needs to be an A+ job to last as long as possible.
A good apicoectomy can not make up for a bad root canal.
Unfortunately I just got the tooth pulled a few days ago it was hurting and I went and seen 2 other dentist and a endo. There was nothing that could be done. I now have the flipper tooth which actually don’t look too bad and it looks natural but it’s really uncomfortable and annoying. I really was upset I had to let my tooth go.
Sounds like you did the right thing.
I am 22 years old and have a huge decision to make and I’m not sure what to do. When I was pregnant with my son last year I developed a tiny cavity on my front tooth. A month after he was born I went to the dentist and he told me I needed a root canal and I was surprised considering how small it was and the fact that it didn’t hurt. He worked me in the schedule that day to do the procedure and I had no idea about root canals and just thought because he was in practice so long he knew what was best. He worked on me and 2 other patients rushing between us. I feel like he rushed through it. Well long story short I went back 3 weeks later because it was still hurting and he said root canals usually hurt for a week or two. He said it was fine and gave me more antibiotics. Also he never put a brown on the tooth just filled it. Approximately 3 months after I developed a pimple above it and still had been experiencing pressure and pain. I went back yet again and he said he couldn’t do anything for it and sent me to a oral surgeon. The oral surgeon said he could preform a apicoectomy and he did. He told me I had a 80% chance of it being successful. Well, 2 months after the apico the pus sack returned so I went back to the oral surgeon. He then again reopened and cleaned and drained the area. He never filled the empty area where the top root was removed just the in side the tooth itself. My tooth is yet again infected and hurting. I went to a new dentist for a second opinion and he said they can do another root canal from the bottom of my tooth and put a crown on it. Do you think it’s honestly worth paying more money getting this 4th procedure or should I just get it extracted? The infection is making my sinus cavity hurt and I feel nauseated a lot. I am a single mother and I’m only going to school. I can’t afford barely anything. I would have to get a flipper tooth and the dentist said the shape of my teeth a flipper might look weird and unnatural but it might be my only option if I have to get the tooth pulled. Thank you for any advice you can give.
Just replied to your other comment
Hi there. I got a root canal (#30) over a year ago and have had reoccurring pain since then. My dentist checked the bite numerous time and basically told me I was fine and just sensitive. Since the root of the tooth way removed I was curious as to why I could still feel my tooth. I have gotten used to the pain of the year thinking it was something I just need to deal with. Trusting my gut I decided to go the Endo who preformed the root canal. With Xrays and a CT scan it was confirmed that the tip of my rootis infected and causing bone loss :(. They recommend an apicoectomy. My gut says no. I don’t know if I should risk nerve damage or just go with the extraction and get an implant. I want the most sustainable option. Since the root canal failed the first time I feel the apicoectomy would fail too. Also I dont really feel like a dead tooth in my mouth is a good option although an implant isn’t real.. idk. I feel like my body is trying to get rid of this tooth. I am doing a round of oregano oil as an antibiotic to see if it helps with the infection and pain. I just don’t know what to do… I’m worried
Also the tooth was root canal after the tooth was rebuilt and crowned. So the crown has actually been drilled through and refilled.
Thank you for taking you time to help.
I really want to take care of this. Im so sick of the constant pain
Can you give me a few more details?
This is a tough call without seeing you.I just noticed that you submitted two comments.
Root canals often fail because the very tip of the tooth may branch out into tiny little nerve endings which cannot be filled by any dentist. Despite having excellent treatment, not all treatment is successful long-term whether that be a root canal or even a dental implant. If the root canal is well done, an apicoectomy may be useful as long as the crown is solid.
Should you decide to have an apicoectomy I would have a simultaneous bone graft so that a whole is not left behind.
before you decide to extract the tooth, make sure you see a very experienced implant dentist to evaluate your bone type for long-term stability.
Good luck
An old root canal was swollen and hurt dentist said it was cracked and sent me to a specialist to try to repair dentist was not able to repair.It has been a year no pain or swelling. Should I do anything,is it doing anything to my health
All teeth that are unhealthy affect your overall health to some degree. There’s no way without seeing you and your x-rays that I can tell you what to do. Make sure you see a really excellent dentist and make good decisions.
Hi. When I was 7 years old I hit my front tooth #8 and the one next to it #7 on a metal slide. This caused my face to constantly swell each day over my check and even causes my eye to be affected.Then when I was 11 years old a blood filled pimple with infection was above the #8 tooth and so I was put on countless antibodies which did not even touch it for about 2 years then I had a root canal on the tooth which did nothing so then I was referred to have a apicoectomy under General anaesthetic on the tooth which was said to be very well done but since antibiotics did not work I was not given any pre op. Soon after the pimple returned in its same place looking the exact same if it worse as I started to get pain so I was then given very high doses of antibiotics hoping that it would blast it and get rid of infection but did not. Then it was re root canal but nothing happened except for the pimple getting aggravated and causing even more pain. It was then decided to have a root canal on the tooth next to it #7 it was done really well but still no joy. Then it was decided to have the #8 tooth removed and a plastic denture to replace it which I still have now until they got rid of the pimple so that I might be able to have an implant. When I was 14 it was decided to have an exploration under general anaesthetic around the area nothing was discovered except for fibrous tissue. Then I had a 3d scan which showed a cyst above the #7 tooth. After that it was decided to have a re root canal on that tooth which took about 6/7 appointments due to the fact they wanted to keep cleaning it out which only made it worse causing it to be extremely painful when talking and eating and a strange new itchy feeling around the area. Once this did not work once again I was told that an apicoectomy was the next step and this is were I am now I know I need it but I am 16 years old and want to know what damage it could have already done to my bone and the area plus I need information about implants and can I have one which are the consequences of everything and will this ever be solved. Please help I fear that this endless nightmare will never end.
You are possibly too young to have a dental implant. I would suggest waiting until you are between 18 and 20 years old if at all possible. Implants are possible in a 16-year-old, but very careful analysis of your growth is required.
Very critical evaluation by 3-D scan would be the most important thing. Some people have a bone anatomy that is not conducive to dental implants and makes apicoectomy procedure very difficult and/or unsuccessful. Lot of this will depend on the thickness of the outer wall of bone and how close the apex of the roots are to the base of your nose. These are things I cannot answer for you via the web without a clinical examination with a 3-D scan.
An apicoectomy can be very successful as long as the root canal itself is well done and there are no fractures. You should not have to live with pain constantly. Once resolved, your teeth should be very comfortable and pain free.
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi, I had a root canal treatment 5 years back and when I checked the doc yesterday he said that the root canal was not performed perfectly and so it formed pus inside the gum.He said that reroot canal is not possible and the tooth will fall off.I want to know whether this pus will affect the remaining teeth and what are will happen if I just leave it coz it’s been 5 years and I have no pain or any thing….thx in advance
Infections are often present without pain. If you just leave it alone, it will become a problem. It will destroy the surrounding bone as the infection festers. It may damage your other teeth too. I see this every day.
If it can’t be saved, remove it.
thx for taking your time to reply 🙂
Please contact me at 407-656-3107 T
hank you!
Hi Erin,
This was found in spam…please call the office if you need to speak to us.
What if the root canal that I got done another tooth grows there but it’s all black what would happen
I am sorry…I do not understand what you are saying….can you re-write this?
😉 Dr. Amin
I would need more information such as x-rays and and exam to help you ..I am sorry
;-(
Hi, Ramsey!
A week ago, my dentist told me after being xrayed that the abscess has extended to other tissues and so I have several options for treatment. One option was to save the tooth (upper front ) by undergoing RCT, then apicoapectomy, then a crown. My second option was to just have the tooth extracted, then a fixed bridge or an implant. I chose the second option because two surgeries really sounded scary. So, I just got my tooth extracted, and will hopefully have the fixed bridge when it heals. But I read from the internet that the abscess has to be scraped off first or something before getting the bridge. My question is, I haven’t undergone or my dentist has not yet performed that. Is that something that I should be concerned about? What if I get the fixed bridge without having to remove the abscess from the surrounding tissues? I am starting to think that the antibiotic that was prescribed will take care of that.
Thank you, Ramsey! I am desperate for answers.
Sincerely,
Kris
Hello Kris,
You will be fine. Scraping the bone is something every single dentist and United States is trained to do. It is nothing unique or out of the ordinary. If there is any inflamed/infected/dead tissue in the socket a curette is used to scoop it out.
Guide is given your wonderful immune system that will take care of the rest. We do not need to worry about anything at all unless he had some sort of unusual infection with bacteria that are out of the ordinary.
Respectfully,
Ramsey Amin DDS
Hi Dr. Ramsey,
Thank you, this article was really informative. However, I still have some questions no one will answer. About 10 yrs ago I had a root canal on my #3 tooth and they also crowned it. In January this year it managed to get infected. I didn’t have dental insurance at the time to I went to a dentist a friend of mine works for and they gave me stronger antibiotics and told me once my ins. Kicks in get a retreat on that tooth. I waited instead, should’ve listened. Then it got an absess on the gum after those antibiotics. I ended up getting a apico done Mar 30. After he sewed me up he said, when he opened the gum I had no bone to drill to get to the root and I would probably lose the tooth anyway but he would make that decision in 6 months when I come back. Once the stitches fell out about 2 weeks later a piece of bone was poking out around the stitch site. It took over a week to come out on its own. Already have an appt scheduled to have to tooth pulled but, oddly enough that tooth is still sensitive to hot and cold. Also the dent in my gum is creepy leaving some of the top of the crown exposed. Not sure if I needed to tell the story sorry. My questions are will I have any of that bone grow back? Is this the beginning of years of gum and teeth issues?
Ugh…you will definitely need one or two stages of bone grafting to reconstruct this area to last 20+years. You may need a sinus lift too depending on your anatomy.
As long as this is done well, you are unlikely to have long term issues. Find a REALLY good DDS to handle this. It will be complex.
This should help you understand the sinus.
https://www.burbankdentalimplants.com/upper-molarinternal-sinus-lift-3-d-scan-real-time-dental-implant-before-and-after-planning-video-narrated-by-ramsey-amin-dds/
RA.
I meant “dull ache” not ” full ache”
Hi,
I had root canal done by my general dentist and it didn’t work. A month later I had endo worked on the same tooth. It was much better but when I pushed or tapped on one side of my tooth (#30) it hurt. I can chew on soft food only. Everyday I have full ache several times a day but it only last for less than a minute. My doctor said my tissue around the apical puff didn’t heal and didnt embrace the foreign object. The x-Ray shown the puff was the same size since 6 months ago. He suggested to have an epico, I am not in much pain and don’t have any infection before/after root canal. It’s been almost 6 months since I had my first tooth canal from my general dentist. Any advise? Thanks
Before considering an apicoectomy, make sure that the root canal is extremely well done. I would evaluate the root canal by 3-D scan to make sure all canals are filled and there is no evidence of fracture.
Apicoectomy’s can be successful when the root canal is perfectly done. If it is not perfect, I would not do the procedure. The root canal system at the very apex is complex and there are thousands of little root canals at the end of the root. The apicoectomy can remove the final bit of nerve tissue that may be causing all of this problem.
Without seeing you it is impossible for me to tell you what to do exactly.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi there,
I had congenitally missing laterals, and had braces and eventually I got implants. before the implants I made the decision to get veneers on my two front teeth and eye teeth to enhance the cosmetics. Ever since I got my permanent crowns on my laterals, my front teeth are shaking. I have told my dentist and he assures me its all in my head. I know something is truly wrong because it has been over a year now, and I am forced to wear a clear retainer daily with no relief. I’m scared to lose my two front teeth and although they look very pretty, they are uncomfortable, loose, and my day to day life is affected. There is no pain, just discomfort, but I’m noticing my gums are starting to rapidly recede, and its making all the money I have drained seem less worth it. Do you think I should get a second opinion from a different dentist? Aside from that, I am 23 and otherwise perfectly healthy. Any insight will help, as it is taking over my every thought and unfortunately consuming my life at this point. I’m tired of being told I’m crazy by a dentist. Lol.
I should also let you know that my bite as been adjusted numerous times and there is no contact in natural chewing. I have a clenching habit I can’t break, and so I sleep with a guard in. The one thing my dentist and I decided it might be is that my guard and my retainer aren’t the exact same, and therefore causing the tooth to move forward with the guard and backward with the retainer. after ditching the guard and using just the retainer for two weeks, nothing changed.
Hi Kaila,
Your bite is the most likely culprit. I understand you had your bite adjusted several times, but that does not mean that your bite functions perfectly well. When we chew or mouth goes from side to side in that must be evaluated also. You likely have a habit were you protrude your teeth subconsciously an edge to edge fashion. Millions of people do this. It leads to wear and mobility of teeth.
Some people just clench their teeth and have a condition called fremitus. This means your teeth are moving while your clenching instead of being rock solid. The periodontal ligament becomes inflamed and the teeth continue to feel looseness.
Find a dental implant specialist with credentials similar to mine in your area. They should be able to work out the problem. Play close attention to your own habits, I’m willing to bet that you clench your teeth or push them into an awkward position that you are completely unaware of.
GRINDING
Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
see answer on next post
Hello, I’m in desperate need of advice about what to do with #14 tooth. Had a root canal about 8 years ago, had to have it retreated due to still having pain, then just last year had another retreatment by an endodontist who found there were more canals that had been missed in the first two treatments. Went and had the pemanent filling put in last week and a couple days later it started hurting so went back to endodontist and the x-Ray showed a dark spot which they said was probably infection & gave me 3 options….apicoectomy, extraction & implant, extraction & bridge. I just Dont know what to do because they won’t tell me if they think apicoectomy will be a success they just say there’s no guarantee. I already have $4500 in this tooth so to risk putting more into it for something I don’t know will work makes me sick! Would you recommend just pulling it at this point and doing an implant or chancing the apicoectomy? Please any advice would be great!
Thanks
Hi Deelea,
I just did an apicoectomy and simultaneous bone graft about 2 days ago. As I have stated in previous comments, the root canal itself has to be perfect in order for an apicoectomy to be successful. Apicoectomy procedure works as long as the root canal is good. You cannot cover up a bad root canal or multiple missed canals with an apicoectomy. They are typically more successful in front teeth than they are in the back teeth. This is because front teeth typically only have one root and 1 canal while back teeth have multiple root and multiple canals and sometimes extra canals called accessory canals.
A dental implant long-term may be your best solution but of course I would need to see you to be able to tell you that with any degree of certainty. The human body, medical and dental procedures cannot be guaranteed…. It is illegal to do so…. Only God knows! Good luck.
If you end up needing an implant, you may end up needing a minor internal sinus lift. This video, 3-D analysis will help you understand the process better.
Upper Molar/Internal Sinus Lift 3-D Scan Real Time Dental Implant Before and After Planning Video –Narrated by Ramsey Amin DDS
Socket Bone Grafting….Do I Need It for My Dental Implant? Ramsey Amin DDS Reviews
Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Happy New Year! I’d like to compliment you on this very informative article about Root Canal Apicoectomy Failure. I have had two treats on the same tooth. My question is: I now have a pimple on my gum. Does this mean I need another treatment? I have Rheumtoide Arthritis and take the necessary medication. Will this effect the treatment. Thank you for your time. All the best for the New Year!
Hi Clover,
Thank you for your very kind words.
Your rheumatoid arthritis is not likely the cause of failure. After two retreats on the same tooth, you are likely better off to remove the tooth.
The pimple on your gums is called a fistula, it is draining a chronic infection which cannot be treated with antibiotics.
Depending on the location of your tooth, it may be possible to do a simultaneous extraction/bone graft/implant/connected temporary on the same visit. I would suggest you have a 3-D scan prior to removing the tooth to determine how much bone is present on the outer wall and how much bone destruction has occurred from this chronic infection and multiple dental procedures on the same tooth.
Antibiotics for a Tooth Infection, Dental Implant, Bone Graft… Do I Need Them?
3d planning example
Good Luck,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi Dr.
I had RCT in both lower frontal tooth 10 years ago, around 5 years ago I got Re-RCT done in one of the tooth and crowns on both.
Now the Re-RCT tooth has developed infection.
I have consulted two dentists, one have suggested and immediate apico with bone graft filling. While other have suggested removal of crown by cutting the crown and re-doing RCT.
I am confused over which way to go. As removing crowns may cause damage to little tooth left post crowning.
And I have read somewhere over web that apico without RCT is not a long lasting solution. Please suggest.
In order for an apicoectomy to be successful, the root canal must be excellent. You cannot do an apicoectomy on a poorly done root canal. The root canal filling must be very dense in the bottom half of the root and all canals must be filled. So the bottom line is that your dentist must evaluate the quality of the existing root canal prior to doing the apicoectomy. If the root canal has problems, retreating the root canal may solve the problem without ever having to do an apicoectomy or a dental implant!!!
Good luck!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I had a root canal that failed and an apico was done on the tooth. Years later it has failed and the tooth was recently extracted (there was an abcess). The site where the tooth was pulled has healed and seems ok, and I am supposed to have a bridge placed soon. I am wondering though – I do have a pimple like area on the jaw area that has been around for a long time. A little sore. Do I need to have this addressed before the bridge? Also what would the original apico have been filled with? I have a strange taste in my mouth and am wondering if when the tooth was extracted whatever was used as filling might have been exposed. FInally, is the apico filling material all removed when the tooth is removed or not? I assume not what was placed in the jaw? Let me know your thoughts. Thanks!
Hello DM,
The pimple that you mentioned is call the fistula. Yes it needs to be addressed before the bridge is done. In fact I would not connect a bridge to this tooth at all. Have a dental implant or several of them instead. Leave this tooth as an isolated tooth. This way if you have a future problem it can be dealt with independently rather than attached to an entire bridge.
Dental Implant or Root Canal – Cost and Value Comparison
Apicoectomy’s of the past used to be filled with amalgam. That is silver filling material. More commonly today the end of the root is filled with MTA which is mineral trioxide aggregate. The other very common and what I feel is the best is no filler at all. The whole should be filled in with bone grafting material such as cadaver and/or cow bone. The root canal must be very well sealed at the apex with gutta-percha. If the pre-existing root canal is not good, the apicoectomy will fail. The crown must also be excellent.
Dental Implant Bone Grafting –Do I Need It?
Generally speaking, when the tooth with an apicoectomy is removed, if there was a filling at the end of the root it typically comes out with the tooth. Occasionally they cannot be found. It is difficult if not impossible to locate without destroying a whole bunch of jawbone if that piece is missing.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
When I was 9 yrs old I broke my 2 front teeth in an accident. I root canal was preformed. When I was 20 the teeth became infected and a 2nd root canal was done. When I was 44 I was having a routine cleaning and my dentist discovered a fistula on my gum. The bone was infected and my front right tooth was removed. Because the bone crumbled when the post was removed my dentist did a bone graft and I had a 6 tooth fixed bridge. This year I developed a pimple in my right nostril that would not go away. My dentist said I had another infection. I had root canal on the tooth next to my missing tooth but the endontist was unable to do the 2nd root canal as he said it was too high up and there was a lot of infection. I was referred to an oral surgeon who preformed a double apico on teeth 9 and 10. Three months later the pimple was back in my nose. My primary doctor sent me to an infection doctor. They did a cat scan with dye and found pockets of infection. I was placed on a pic line with 24 hr antibiotic infusion for 6 weeks. 5 weeks in a became septic and ended up in the hospital for over a week. While in the hospital my gallbladder failed and had to be removed and my occipital nerves became inflamed. I continued on oral antibiotics for a couple of weeks after being released from the hospital. This was in July. Last week the pimple in my nose started back no too sore but I feel pressure. Today my dentist said the apico looks good on xray but he wants me to go back to the oral surgeon do to my history. Any ideas?
Hello Kathy,
Jeez…I feel so bad for you. This is not typical at all!
I would suggest that you have a 3D scan taken of your whole mouth. This will allow for discvovery of most if not all of the hidden problems in your mouth. A 3-dimensional scan allows you to look behind roots and over the top of your roots. Failing apicoectomy’s, failing root canals can be seen very easily on a 3-D scan of high resolution. More importantly, the dentist ability to read the scan is critical also. Some dentists look at 3-D scans every single day over the last decade while some only occasionally review a 3-D scan. It may actually be helpful for you to have a second person such as an oral maxillofacial radiologist look at your scan too.
Upper Molar/Internal Sinus Lift 3-D Scan Real Time Dental Implant Before and After Planning Video –Narrated by Ramsey Amin DDS
3D Scan
The apicoectomy procedure is not a bad procedure. When indicated, an apicoectomy can be done very successfully. The key is choosing the right teeth to do an apicoectomy on. In my opinion there are very few teeth that apicoectomy’s can work. They should always be done in conjunction with a bone graft in my opinion. I do apicoectomy procedures on teeth that would only be perfect candidate for successful outcomes.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Please help me! I’m miserable in pain on #11 for exactly 9 months. I have constant pain. The 3D scan by J Morita showed a horizontal line at the tip of the metal post 8 months ago. I was told it’s an artifact. X-rays didn’t show any problems. 6 months ago I had an apicoectomy done. The doctor said there was a little bit of of granulation tissue but the tooth is good. As of today, I don’t want to live anymore. That’s how bad the pain is. And I have constant nose swelling as well. Dentists say there are no changed in bone, tooth is good. But why does it hurt so much for such a long time? I just did another CT scan by Galileos CT and it does’t show any fracture. What should I do? Should I believe the J Morita CT?
Hello Yelena,
So sorry to hear about your constant pain. If the tooth has a root canal and a post and you have had pain for 9 months it is likely fractured regardless of what both of your scans show.
In order for a fracture to show up on a scan, the size and width of the fracture must be large enough to be seen by the resolution of the scanner. A tiny crack can cause a ton of pain which will not show up on the 3-D scan until much later. If the pain is localized to tooth #11, I would have it extracted and have a socket bone graft done on the same day of extraction. I would not place any immediate implant into this area until all of your pain has gone away.
Using platelet rich fibrin (PRF) will help the extraction process tremendously.
I’m assuming the crown has been taken off to evaluate it visually for a fracture. Apicoectomy procedure does not fix fractured teeth. The only treatment for a vertical fracture is extraction and replacement with a dental implant.
Socket Bone Grafting….Do I Need It for My Dental Implant? Ramsey Amin DDS Reviews
Burbank Dental Implant Specialist: Review of Immediate Dental Implant Considerations
Cone Beam 3D Scan X-ray – Basics For Dental Implants
Do I Need PRP/PRF/PDGF/BMP For Dental Implants and Bone grafts?
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dr. Ramsey,
I had an apicoectomy done about 3 months ago. At my checkup today, the spot was still dark and looked almost the same as it did 3 months ago, just rounder from the recent apicoectomy. Isn’t it supposed to be healed by now? He said it could take about a year to heal.
Hello Nick,
If you had a bone graft done at the same time as the apicoectomy the area should look fairly uniform on x-ray at this point. If you did not have a bone graft, then the area may still look dark. Of course these are generalizations without having seen your x-ray.
When I perform an apicoectomy, there is always a bone graft done in conjunction with platelet rich fibrin –PRF — I take an x-ray before the patient leaves. The x-ray looks completely uniform on the day of the procedure before the patient leaves the office. Find out if you had a bone graft done.
Bone Grafting For Dental Implants…Where Do You Get the Bone?
Do I Need PRP/PRF/PDGF/BMP For Dental Implants and Bone grafts?
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi Dr Ramsey,
I have a serious dilemma on my hands. My upper left canine had a RCT 10 years ago (I’m 35) and now shows a large periapical infection. Here is the x-ray: http://i.imgur.com/zIUjQBZ.jpg
The Endo attempted to redo it, but said the cement is too hard and left it as is. He suggested I do an apicoectomy and remove 5mm of the root.
Do you think this is a wise move, even if he could not redo the RCT? When I suggested extraction, he said that the upper canine is very important and my face would lose its shape on one side if I do it, even with an implant.
What do you think is the wisest move?
Hi James,
Somehow your comment got lost as spam…. Probably due to the link that was embedded…. Sorry.
An apicoectomy cannot replace a bad root canal. I would suggest finding another endodontist I can retreat the root canal before doing an apicoectomy. If you just cut the root off, I think you will still end up with a problem in the future. All of the apicoectomy’s are performed are done with bone grafting and platelet rich fibrin/PRF. I have not seen a failure in many years but I choose my cases very wisely. Only about 5% of failing root canals qualify for an apicoectomy and they are generally front teeth like yours. The gutta-percha at the end of must be very sealed and no retrofill is necessary.
Do I Need PRP/PRF/PDGF/BMP For Dental Implants and Bone grafts?
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
hello doctor,
I had a root canal on a molar tooth last year…one week back I saw a pimple…after x ray doc found a crack…he retreated it n d swelling was gone…today on d second session he did a filling n I now can sense swelling again..is it curable?
Hello Pari,
If the tooth is cracked, there is a good chance that he needs to be extracted and there is no cure.
Sometimes a 3-D scan can visualize a fracture that cannot be seen in your mouth her on traditional dental x-ray.
This link will show you what type of imagery you can see on 3-D scan.
Upper Molar/Internal Sinus Lift 3-D Scan Real Time Dental Implant Before and After Planning Video –Narrated by Ramsey Amin DDS
Very respectfully,
Ramsey Amin DDS
Diplomate of the American Board of Oral Implantology/Implant Dentistry
Fellow of the American Academy of Implant Dentistry
Burbank, California
Dear Doctor:
I had an upper molar pulled this past week. It came out in pieces and I felt the dentist pulling the tooth out by leaning his tool against my open lips. I now have an inch long raised and sensitive area of gum that could well be bone above the outer part of my former tooth socket on the side that the dentist did all the pulling. It feels like my gums are stretched to accommodate what may be bent or pushed in bone.. The dentist involved saw me the next day and said I should heal fine. An xray showed that there was no trace of my pulled tooth in my socket.
Is my pushed up gum and possible “bent” bone normal?
Thanks.
Hello Alson,
My guess is you lost bone on the extraction. This could either be due to the tooth being so bad that the bone dissolved away. Or it could be due to the bone being connected to the tooth as it was extracted.
Regardless, if this was an upper molar, he will likely need a bone graft at the time the implant is placed. Sometimes internal sinus lift is required also for an upper first or second molar.
Bone that is bent in is a sign of bone atrophy or lack of bone volume. Either way, this dent will need to be repaired if you’re having an implant placed.
Upper Molar/Internal Sinus Lift 3-D Scan Real Time Dental Implant Before and After Planning Video –Narrated by Ramsey Amin DDS
Socket Bone Grafting….Do I Need It for My Dental Implant? Ramsey Amin DDS Reviews
Very Respectfully,
Ramsey Amin DDS
Diplomate of the American Board of Oral Implantology/Implant Dentistry
Fellow of the American Academy of Implant Dentistry
Burbank, California
Hello this is Jennifer Clark, I had a root canal done 4 years ago and right after I had it done it chipped. I went to the dentist and they said that i need another root canal. I dont have any pain or swelling in the tooth and it is my front tooth. I dont want to have it taken out. I just want to know what I should do. Should I have another root canal done or should I get another opinion.
Thank you so much
Jennifer Clark
Hello Jennifer,
My guess is you have what is called a periapical radiolucency above a tooth that is completely without symptoms. This means that the root canal never completely healed or has become reinfected. This can be due to a crack in the root or a canal that was not filled or even an extra canal. Some canals cannot be even found by any dentist.
If it is left alone, it will get larger, you will lose more bone and eventually you may lose the entire tooth. Unfortunately these things come without any symptoms for you to be completely aware of them.
Very Respectfully,
Ramsey Amin DDS
Diplomate of the American Board of Oral Implantology/Implant Dentistry
Fellow of the American Academy of Implant Dentistry
Burbank, California
Dear Dr. Amin,
About three months ago I had an apicoectomy on a lower left molar (19?) on an infection that resulted from a 10+ year old root canal with crown. Since the apico, there has been a large hard bump closer to the jawline that has not gotten smaller, nor does it seem to get bigger.
I was not concerned in the beginning because I knew that healing from the apico takes several months and thought also that the bump would be maybe scar tissue? (is this possible?)
However, the bump is sensitive (not painful or maybe I have a higher tolerance for pain) and the tooth area still has some sensitivity to it.
I returned to the Dentist who said the x-rays show that the bone seems to be healing normally, but the bump is indicating a problem. I am on antibiotics for 10 days and will get a tooth extraction, bone graft and implant in 3 weeks. Is this span of time ok to wait? Unfortunately I am traveling can cannot have the surgery sooner.
I am nervous about the situation and have a few questions.
Should the bump go down while taking the antibiotics? And how soon should I see results to see if it is working? Also, will this extraction solve the current problem and what are some questions or concerns I should have from an already compromised area?
Finally, I am allergic to nickel and propylene glycol and was wondering if any of the extraction/implant/crown procedure will contain these materials.
Thank you for your time, article, help and prompt responses to everyone’s post!
Best regards,
Esther
Hello Esther,
The bump may or may not go down while you’re taking antibiotics. The extractions should solve the current problem as long as the bone is filled in properly. Of course you have to heal very well too. The area has been compromised by multiple surgeries and bone loss from chronic inflammatory and infectious processes. This dental implant will just take more time then perhaps one that could be done in one visit. I would suggest going very slow and taking the time through every stage.
Nickel is present in some nonprecious metals. Titanium and titanium alloy dental implants do not contain nickel. I would make sure your implant crown is all ceramic such as E max in the front of the mouth or monolithic zirconia if it is in the back of the mouth. Propylene glycol is not used in dentistry.
Sorry for the delay in responding to your question. I’m just catching up after the Thanksgiving holiday feast!
Ramsey Amin DDS Reviews Solid Zirconia Custom Dental Implant Crowns and Abutments Instead of Metal
11 Considerations for Full Porcelain Dental Implant Crown Materials –Review by Burbank’s Ramsey Amin, DDS
Very Respectfully,
Ramsey Amin, DDS
Diplomate of the American Board of Oral Implantology/Implant Dentistry
Fellow of the American Academy of Implant Dentistry
Burbank, California
hey my name is karina 🙂 and im 16 …….i had a root canal a while ago when i was like 9 …… and years ago it started to like break like the feelingg broke little by little i was soo scared to go and now im just left with a tooth like in the gum and its like nasty looking right when the whole feeling came out it had stuff down in it .. but the tooth is just down in the gum but you can still see it im soo scared of the dentist do you know what there gonna do for that? :'( please reply
Hello Tara (Karina)
It sounds like your tooth is going to have to be extracted. It would be very easy to have this done while you are sedated. The whole procedure can be done while you sleep under moderate IV sedation. It should feel like 1 minute one by.
Get connected with a dentist that can sedate you under IV… And of course, speak to your parents ASAP.
Details of Sedation
Very Respectfully,
Ramsey Amin, DDS
Diplomate of the American Board of Oral Implantology/Implant Dentistry
Fellow of the American Academy of Implant Dentistry
Burbank, California
I had pain in my tooth #6. My dentist did a root canal. I still had pain so he did another root canal. I still had pain so we did an apicoectomy. I was still in pain so off to the oral surgeon. He extracted it and I had a dental implant. I was pain free, then my dentist tried to load it (after the go standard healing time). I had to have the crown ground off because it was painful. When the crown was taken off my gum was raw and bleeding underneath. (Like the crown had been rubbing on my gum) I had the healing collar put back on and no pain. We have tried to load the implant several times over the last 7 months and each time it hurt. I went to a prosthodontist who said and I quote “it’s a mystery”. The latest problem is my implant has started hurting even with the healing collar on so I had my dentist take that off and it still hurts. This pain is a little different, it’s more of a deep, constant pain, not the surface pain of before. I am at a loss! How do I know if the implant has failed? If it has failed what do I do now? If it hasn’t failed, what do I do now? I have been dealing with this for almost 3 years and I feel like the only one who listens is my dentist but he is at a loss. Thank you so much for your time!
Dear Janet,
What you describe is extremely odd and not normal whatsoever. I would suggest you take a 3-D scan of the implant and make sure there is bone 360° around the entire implant. My guess is that your implant is probably partially integrated and perhaps has some sort avoid or dead necrotic area. Keep me posted as this is unusual to have a crown taken on and off like you described.
A 3-D scan can see what a regular x-ray cannot.
3D Scan
Dental CT Scans and Bone Width For Implants – Burbank Implant Expert Explains
Very respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hello,
I have a long history with a failing root canal. I had root canals done on teeth number 9 and teeth number 10 when I was 12 (trampoline accident). When I was 17 these root canals failed and I had apicoectomy surgery on both teeth. I am now 22 and this past June had to have yet another apicoectomy because the first one failed. I now feel a burning sensation and believe it is infected AGAIN. I have an appointment with an oral surgeon tomorrow but can anyone give me some advice. I am about to just get the teeth pulled and get implants because I am so frustrated. Similar infection problems don’t happen with implants, do they? Thanks!
Dear Maggie,
Sounds like these teeth have been causing you trouble for a long time. Similar infections do not happen with dental implants. You can develop an infection around an implant called peri-implantitis but this does not occur commonly and is the exception rather than the rule.
In order for an apicoectomy to be successful the root canal and the crown buildup must be perfect.
Too many times the reason why apicoectomies fail is because the root canal itself is not perfect and the apicoectomy is done anyway. And if the crown is not perfectly sealed, all of this will leak bacteria through the gutta-percha filling and back into the bone causing another apicoectomy failure.
Be sure to have a bone graft done when you remove a tooth that has an apicoectomy in the front of the mouth. It is extremely likely that you already have bone loss that will need to be corrected in order to have a well placed dental implant that will serve you for many many many many years!
Socket Bone Grafting….Do I Need It for My Dental Implant? Ramsey Amin DDS Reviews
Very respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I have a question, I’m 20 years old, I had two root canals and two crowns put on my two front teeth.One of these tooth have re root canal done and also apicoectomy done…now both these teeth don’t have pain but they have mobility… when my tongue touches these teeth,i feel that they are a bit shaking…and they have mobility…what should I do???will I have to undergo RCT again…or I’ll have to get it extracted… 🙁
.please reply…. I’m in urgent need of the answer…
Dear Chitra,
Don’t rush off and have these teeth extracted for dental implants or have root canal treatment!!
The most important thing is that the bite is adjusted so that there is no trauma to the teeth during natural chewing. The teeth should be “taken out of occlusion” or taken out of bite by your dentist. If the teeth are mobile during the healing phase, there is no way that they will heal well. Especially if a simultaneous apicoectomy and bone graft was done, you need to have ZERO mobility during that initial healing phase. The tooth needs to reform what we call a lamina dura and a periodontal ligament space.
See your dentist ASAP and make sure the teeth have no bite. This should be a very simple adjustment in can be done in about 5 minutes.
Apicoectomy Failure – Burbank Dental Implants Success Video Testimonial
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
Thank you for the information.
About two and a half years ago, I had a root canal in my front left tooth. After a couple of months, the infection came back and I had to have an apicoectomy. It is now two years after the apico and I am experiencing a large amount of pain and tenderness as well as the bump above my tooth. I have seen a dentist and he informed me that there is no infection and it is probably just irritated.
I am only 19 years old and would like to solve this permanently because of all of the trouble it has already caused. I am interested to hear your opinion and what you think my best option is.
Thank you,
Alyssa
There are times that I do an apicoectomy, but it is always in conjunction with a bone graft simultaneously. In order for an apicoectomy to be successful, the root canal itself has to be excellent and it is often best if the root canal is re-done just prior to the apicoectomy and some of the root canal filling material is sticking out on purpose. This allows the dentist to cut off the end of the root and attain a good seal against bacterial invasion coming through the root.
Just make sure the root canal is really excellent on the tooth with the apicoectomy. If not, it is bound to fail and end up as a dental implant.
I do apicoectomy procedures, but choose each situation very carefully and only do the ones that I feel strongly will be successful.
Unfortunately everything in dentistry and medicine has a lifespan. Even people that get hip and knee replacements have to have those replaced too! They get changed every 10-20 years!
I try to provide services for my patients that will last as long as possible and make sure they understand the long and short term implications of every option.
How Long Have Dental Implants Been Around?
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I am in desperate need of advice! I’m on vacation in Germany, and due to board a ship for 13 nights to head back to the states, and while on board I will have limite or no dental care. My problem is that 2 weeks ago, I developed swelling/pain on my gum beside a molar that has had a root canal (guessing about 10 years ago). I hoped it would go away, but it got worse, so I found a dentist here who took an xray and said it was an infection in the endodonic canal, and he put me on antibiotics for 6 days. Today it’s day 5 and no improvement, I can see a pimple above the swelling. I don’t have pain but it is obviously bothersome. Is it safe to wait until I get back to the states to decide what treatment to do? The dentist here said the other option is extraction, but he seemed sure the antibiotics would work. I have 3 weeks before I will get home. I am worried that I will be doing further damage if I wait, but I only have a week before I board the ship. Any advice you can give would be greatly appreciated!
Hello Rhonda,
Given your situation being on a cruise ship I would suggest 1 main thing.
Switch antibiotics to different antibiotic family or add-on a second antibiotic.
Example: If you’re taking amoxicillin and it is not working then either switch to clindamycin or add metronidazole to the amoxicillin.
The infection may be so significant that the bacteria may be resistant to the type of antibiotic that you’re on currently. The infection may be so bad that you may have to have the tooth extracted or have the area drained if antibiotics do not work at all.
Sorry for taking a few days to get back to you on this. I had over 300 comments to reply to!!! I’m trying to help everyone.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
Hi Ramsey,
it is me again! I posted a msg on July 20, 2014 at 8:22 pm here.. I opted to have the tooth removed, the pain was really excruciating and my parents talked me out of doing the apico. Thing is, the same day my dentist extracted the tooth, I told him I was experiencing some pain on the same molar on the other side (one before the last, bottom right – excuse my layman’s language!). He located huge decay on it and it was so close to the nerve that unfortunately nothing worked: overly failed, crown failed, lowering the crown failed, root canal failed***: I’m back to square one!!!!! It turns out I have 4 canals and it seems one or more are bending and are not reachable=exact same situation as my other former tooth.. I am now thinking whether the anatomy of ALL of my molars* are like this.. because I cannot extract every tooth as they get infected that is awful.. what do you recommend? Shall I go back to my dentist and ask about the anatomy of my other molars – if he says it is the same case with the others – 1. do you then recommend the apico if there is enough outer bone and good root access? Sorry I think you missed a key word in your previous comment: 2. is it easier* to replace an apico molar with an implant than an apico front tooth (eg incisors)? 3. 4. Would I need to stay at home for a week after the operation in case I go down that route? nobody seems to give me a definite answer.
again THANK YOU
Lucy
I have the appt for the implant intervention next Tuesday.. wish me luck I need it!!
MY ANSWERS IN CAPS
1. do you then recommend the apico if there is enough outer bone and good root access? Sorry I think you missed a key word in your previous comment: —I WOULD NEED TO SEE YOU TO ANSWER THIS
2. is it easier* to replace an apico molar with an implant than an apico front tooth (eg incisors)? –YES, typically
4. Would I need to stay at home for a week after the operation in case I go down that route? nobody seems to give me a definite answer. —NOT LIKELY –but everyone heals very differently
______I would suggest you seek an opinion of an endodontist or a general dentist who is very skilled and root canal treatment. (your current dentist to may already be that person!!)
The last thing you want do is save teeth that have a poor prognosis for crown as you will only eventually end up extracting those teeth. I see this every single day multiple times a day… Teeth that were salvaged… That later became extractions.
On another note, you need to work with your dentist and hygienist to learn the prevention to avoid ever needing dental work in the first place. It is way more information than just brushing and flossing.
Be sure to consider socket bone grafting if these are critical areas for dental implant replacement.
Socket Bone Grafting….Do I Need It for My Dental Implant? Ramsey Amin DDS Reviews
Very respectfully,
Ramsey Amin DDS
I have a question, I’m 20 years old, I had two root canals and two crowns put on my two front teeth.One of these tooth have re root canal done and also apicoectomy done…now both these teeth don’t have pain but they have mobility…
when my tongue touches these teeth,i feel that they are a bit shaking…and they have mobility…what should I do???will I have to undergo RCT again…or I’ll have to get it extracted… 🙁
Dear Chitra,
Don’t rush off and have these teeth extracted for dental implants or have root canal treatment!!
The most important thing is that the bite is adjusted so that there is no trauma to the teeth during natural chewing. The teeth should be “taken out of occlusion” or taken out of bite by your dentist. If the teeth are mobile during the healing phase, there is no way that they will heal well. Especially if a simultaneous apicoectomy and bone graft was done, you need to have ZERO mobility during that initial healing phase. The tooth needs to reform what we call a lamina dura and a periodontal ligament space.
See your dentist ASAP and make sure the teeth have no bite. This should be a very simple adjustment in can be done in about 5 minutes.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
thank you so much doctor…. thanks a lot…. 🙂
About 2 months ago my front tooth abcessed. That was the most awful pain ever. The tooth had a root canal some 30 years ago and had since been crowned. After the infection, the dentist did an apicoectomy. Today, I feel like there is still some feeling in that tooth, not really deep pain but a slight nerve pain sensation. Can that tooth re-abcess? I’m so afraid of that happening again.
Hello Christine,
Yes the tooth can develop another abscess. If it does, the long-term prognosis for this poor and you may end up with a dental implant. When the same tooth becomes reinfected, its prognosis for another third retreatment is not very good. Sorry for the bad news
Dental Implant Procedures
Ramsey Amin DDS
Thank you for explaining this! I had a root canal done in my front left tooth about 2-3 years ago. About half a year after the root canal, I began feeling pain and pressure in the tooth. I also had a painful abscess above it. I went to a specialist, who scheduled me for an Apicoectomy.
It is now 2 years later and I am having the same symptoms: a tender, painful tooth and an abscess above my tooth. I am a full time college student and don’t have dental insurance anymore. At the time of the Apicoectomy, I was not aware that this procedure might only be a ‘temporary fix.’ I am currently not sure what steps to take to fix this problem and would love some professional advice!
Thanks,
Alyssa
There are times that I do an apicoectomy, but it is always in conjunction with a bone graft simultaneously. In order for an apicoectomy to be successful, the root canal itself has to be excellent and it is often best if the root canal is re-done just prior to the apicoectomy and some of the root canal filling material is sticking out on purpose. This allows the dentist to cut off the end of the root and attain a good seal against bacterial invasion coming through the root.
Just make sure the root canal is really excellent on the tooth with the apicoectomy. If not, it is bound to fail and end up as a dental implant.
I do apicoectomy procedures, but choose each situation very carefully and only do the ones that I feel strongly will be successful.
Unfortunately everything in dentistry and medicine has a lifespan. Even people that get hip and knee replacements have to have those replaced too! They get changed every 10-20 years!
I try to provide services for my patients that will last as long as possible and make sure they understand the long and short term implications of every option.
How Long Have Dental Implants Been Around?
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hello and thank you for the great information. It is very helpful to read all the experiences.
I have to decide this in 2 days!
I have been approved for apicoectomies on 10 and 11. tooth #10 with a root canal is at the end of an 8 tooth bridge with 2 teeth on each side holding it in (a car accident 30+years ago and subsequent teeth losses). #11 is a single RC/crowned tooth.
1 1/2 years ago I lost my bottom molar on my left side and so chewed more on my right side. All good. Then I lost the last 2 teeth on my right side from a failed RC and fracture under a 3 tooth bridge. The surgeon cut the bridge and left one tooth there. This caused me to start chewing on these 10 and 11 teeth more. They got sore and I went to the dentist and he ground them down a bit and referred me to the oral surgeon. Insurance approved apicoectomies for these 2 teeth. But for the past 4 months I have no pain. It all subsided after I quit biting so hard. Also, there has never been an infection and I have only had pain when I chew a lot on them, like meat or hard veggies. I had some pain in the bridge behind it when I had sinus issues but all of it doesn’t hurt at all now.
The question is, are these apicoectomies necessary? Or should I leave them alone until I would have an infection or some other issues? They are not preventative I suppose or would they improve the life of the teeth?
I really need implants on these bottom molars so I can start to chew where I should chew and take pressure off of these more fragile teeth? Perhaps this is a better investment?
Thank you so much.
Hi Patty,
It is very difficult to tell you whether or not you need these apicoectomies without seeing you and your x-rays. Many dental infections that occur around root canal teeth have no symptoms at all. They will simply show as a black spot at the tip of your root on an x-ray. Most of them are not symptomatic until one day they abscess!!!
If you do have this black spot at the end of your root, this is bone loss and oftentimes an apicoectomy and/or root canal retreatment is indicated. It sounds like you have extensive dental work. I would go with the recommendation of your dentist. Keep in mind that an apicoectomy shortens your roots and may make your bridge looser.
I would not wait on doing treatment. On another note, you should have a complete evaluation for the health of all of your teeth and try to prevent is much possible dentistry by long-term maintenance.
Dental Implant or Root Canal – Cost and Value Comparison
Very respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Deep thanks for your explanation. I have an appointment Sept 10th and will ask all the questions you proposed.
Patty
Hello Dr.
When i was 8 years old my right central incisor was knocked right out of my mouth… with a tree (yup you read that right). Not only this but my upper jaw was broken in several places. The dental surgeon cemented the tooth back into place and wired my upper teeth together. After he was sure that the jaw had healed and that the tooth would stay he began a root canal procedure. It was successful and for years I have had this tooth which was properly crowned later on in life in my early 20’s. I am now 27 and it appears that there is some decay and a crack on the tooth above the gumline. I am scheduled to see a surgeon on Sept 2nd but am wondering how long this tooth can last before I have it taken care of. My only concern is for the teeth around this tooth, the last thing I would want to do is jeapordize the surrounding teeth because I was hesitant to get the root canal tooth done sooner than later. There is some pain (which I find surprising since the tooth is dead). Thank you in advance for any advice and assistance you can offer.
Justin
Hi Justin,
No one knows how long this tooth will last. Given the fact that it had issues such a young age, it is likely that you’re going to lose it. Oftentimes teeth that are traumatized undergo a process called resorption where the tooth literally dissolve away. It can become painful even if the tooth had a root canal.
Your best case scenario would be to replace this tooth with any immediate dental implant considering it is a central incisor. A bone graft will likely need to be done to fill in the void around the tooth socket and the dental implant if it is safe and predictable to be placed on the same day of extraction.
The “Void” Bone Graft for Immediate Single Implants – American Board Diplomate Explains
I know you don’t want to part with your tooth, but it is likely the best case scenario before one day it breaks off entirely. I saw two of these last week alone. It creates quite a cosmetic emergency when your front tooth breaks off to the gumline.
Very respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
A very interesting article! I am looking at a two implant supported bridge at the upper front and have a problem tooth nearby that has a poor history of root canal work. My dentist is advising against the implant until the nearby infected root situation is resolved and has advised extraction rather than re-root canal/apicoectomy. I’m pondering this as it would mean three implants instead of two (more work/more cost!). Your article has made me think again! Still not sure on whether to treat the infection through extraction or leave well alone and stick with the two implant bridge. The infection isn’t problematic as I haven’t had an abcess now for 3 years (I was getting them annually!)
Hello Jim,
I absolutely love your question. Most dental infections are chronic in nature and cannot be felt by the patient. They are picked up on routine dental x-ray examination has a black spot at the tip of the root.
Your dentist is absolutely correct in being extremely hesitant to placing implant next to a tooth that has a long-standing chronic dental infection. Your asking for trouble by doing this. Your asking for your dental implant and/or bone graft to fail because of a type of bacteria that is generally walled off within that abscess/black spot of inflammation on your x-ray. It sounds like your dentist has your best interest in mind.
The health of your dental implants is largely predicted by the health of the natural teeth right next door. Dental Implant or Root Canal – Cost and Value Comparison
Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
hi doctor I just had an apicoectomy don’t about a month ago for the second time. I am suddenly feeling discomfort and swelling. I feel hopeless, I’ve had this done before. But after reading this article having a tooth extracted sounds so painful and I’ve never had a tooth extracted before. I went to see a specialist and he fixed it twice, but it’s only been a month. He never said to come back just to do 2 laser treatments to help heal and to cut stitches. no check up.
Hello Carla,
I would suggest you see your Dr. back for a follow-up visit. In my practice I will see 98% of patients back at a one-week follow-up appointment. At this appointment we can be certain that things are healing properly and that there is no presence of infection. If an infection is present oftentimes a second antibiotic is added or antibiotic therapy is changed altogether with a possible culture and sensitivity to make sure that we are treating with the proper antibiotic.
I do perform apicoectomies, when I know the prognosis will be excellent. This is always combined with a bone graft, membrane, PRF/PRP and sometimes splinting of teeth.
Platelet Rich Plasma (PRP)
Keep us all posted on your situation please.
Very respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
Dear Dr. Amin, I have an infection in my front top tooth that had two failed root canals and now I am told to have an apico by my endo. My main dentist told me before I can get implants I have to get braces to fix my major malloclucion which most likely is the cause of my horribley painful tmj. My tooth has been infected for over a year now and im growing quite concerened over bone loss which my endo told me I have. Should I wait to get implants for braces? Would MMS help to stop with the infection? Thank you.
Hello Mel,
After 2 failed root canals, an apicoectomy may not have a high success rate in your situation. I in fact do perform apicoectomy is when I know the prognosis will be excellent. These are generally for single rooted front teeth and not for molars.
MMS is some type of homeotherapy I believe that is not likely to be successful. In order to go through your dental reconstruction, your TMJ problems must be absent in your bite should be comfortable prior to starting any implants or significant restorative dentistry. A decision needs to be made soon whether or not this tooth should come out. Braces need to happen prior to dental implants since dental implants cannot move.
https://www.burbankdentalimplants.com/full-mouth-restoration/
Very respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
Hey Doc,
I had an apico on one of my front lower teeth 9 years ago. In all the x-rays I’ve seen since then i’ve always seen a dark area by the tooth but it never seemed to get bigger and my dentist never made it an issue. However, I’ve just relocated and went to a new dentist who had an endodontist check it out who x-rayed it and said I need apico again. I have a few concerns:
It’s my front bottom tooth which is already small to begin with. Is doing another apico going to make it looser?
Also, since there is still that dark circle by where they did the apico before, does that mean its re-infected since I thought it was normal after an apico to have a dark shaded area like that.
Please advise and thank you.
Hello Nick,
There should be no dark spots on the x-ray near the roots. When I do an apicoectomy, I always bone graft the hole in use the patient’s own blood to make the graft successful.
If the root a short and mobile, it may need to be splinted to the other teeth so that it doesn’t move during bone graft healing. Lower front teeth are very tiny by their nature.
Good luck, I hope it really works out for your this time!
Here’s some information about bone grafting that you should know:
PRP – For Accelerated Healing Of Dental Implant Procedures
Very respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
Dear Dr. Amin,
I have read all posts here.. really feel sorry for all of these folks, including myself. I have had root canal treatment (4 sessions over a period of 1.5 months) on my lower left molar (second to last) with a total of 3 dentists on the same clinic, and the pain never went away completely. I had a CT scan done yesterday after talking to my dentist on the options.
My dentists all said I have curved canals and showed me on the x ray they could not reach the tip of the root. Some recommended apicoectomy, however here is my dilemma: if the success rate for apico is not very high and the tooth may end up getting extracted down the road.. is it worth trying this?? Of course this will depend on how close to the nerve it is, root length, etc.. but I read from you that bone is extracted to reach the roots and it seems to be an aggressive intervention, which might cause the implant to cause problems in the future once I have it done? I do not think that an apico might be a good option because (1) it is so invasive requiring bone to be drilled, which may cause issues with implants and (2) there is 60% chance of success.. I will see the results of the CT scan with the dentist tomorrow. If he says conditions are okay for an apico, (a) what would you recommend? I find the idea of drilling through my bone, cutting through my gums and having the tip of my roots extracted for a 60% success rate not that much attractive compared to an implant after all. However (b) how long do implants last for? I am only 27 and would need the implant to last for many many years to come.. Thanks for answering to question (a) and (b)
Hello Lucy!
I would recommend that you be evaluated with the 3-D scan. If the outer wall of bone is of reasonable thickness and the route is accessible, then apicoectomy may give you many years of good service. Some apicoectomies work great!
If they feel like the prognosis is good, then by all means proceed. It is much replace a molar on the lower left that has had an apicoectomy with a dental implant than an upper front tooth that has had an apicoectomy.
Dental implants are the closest thing to your natural teeth, and just like us, we don’t live forever either. A dental implant may have a lifespan from 10 to 40 years. It depends on a number of factors in there are a few ways to predict success.
https://www.burbankdentalimplants.com/disadvantages-of-dental-implants-the-cons/
Good luck with everything… I’m sure it will turn out well! 😉
Very respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, CA
Dear Dr. Amin,
I’m desperate for an answer. In April I started experiencing swelling on the roof of my mouth near an upper molar. My DDS diagnosed the swelling as an abscess. I was referred to an endodontist who performed an initial root canal. The abscess never subsided. After a second visit, the endodontist said he made “a few adjustments.” Again the abscess never decreased in size. After a third root canal (and the final treatment), the endodontist assured me the tooth was healed. At the time of treatment the abscess had developed into something that resembled a pimple. He punctured it using a syringe and I was told that it should heal. However, it is now three weeks later and the abscess still persists (in fact, it hasn’t changed much since the initial treatment). Do my symptoms indicate that I still have an infection? I can’t find an answer, and I’m uncertain what to do at this point. I’m totally frustrated.
Any insight you could provide would be tremendously helpful!
Thank you in advance!
Amanda
Hi Amanda,
There is a strong possibility that one of your teeth next to this tooth is also dying or dead. Please have your endodontist test that tooth to see whether it is alive or dead.
Another common thing that occurs is the root canal tooth fractured vertically. If that is the case the tooth will have to be extracted and subsequently replaced with a dental implant. Lastly, additional nerve canals are sometimes missed in upper molars that can lead to a reinfection and secondary abscess.
Keep me posted with what happens. I understand your frustration. Hang in there. The human body can sometimes be unpredictable!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I had a rood canal on my front top left tooth over 20 years ago. About 6 months ago I started to develop pain and discomfort in the area, as well as constant headaches. I was referred to an endodontist who redid the root canal and performed an apicoectomy. In the last 2-3 weeks I have started feeling discomfort in the area again as well as headaches. I will be going in next week to see the endodontist, but I am worried about future problems and possible bone loss. How common is it that significant bone loss in that area would complicate treatment, and would repeated root canals and apicoectomies result in more bone loss than simply opting for extraction and implant at this point?
Hello Shelley,
Repeated apicoectomy’s would definitely results and more bone loss. Repeated root canals may or may not result in additional bone loss. There only so many times that you can reenter the same tooth and area before there is still a little tooth structure left that a crown would not end up lasting that long. You need to way the pros and cons with a very skilled and experienced implant dentist and endodontist. Only then after a very detailed examination and possible 3-dimensional scan, can you make a really good determination for the longevity of each option.
Attached is a link to learn more about 3-dimensional scans https://www.burbankdentalimplants.com/cone-beam-3d-ct-scan-x-ray-basics-for-dental-implants/
best of luck to you… Ramsey Amin DDS
I recently read the article on a failed apicoectomy. I have had two crown replacements on #3, upper right arch; a total of 3 crowns. An endodontist recently recommended doing an reverse root canal to target the 4th root canal and to then do another apicoectomy. According to your article, there is only a 40% success rate. How would we find out if the tooth is viable after all this time to do the above recommended? I really want to save my tooth!! I’m moving to another state in 2 months and I’m trying to figure out if it’s best to get it done now or just go with an implant where I move to…..
Hello Raquel,
Some apicoectomies can last a long time if the tooth has a good prognosis after the procedure is done. The apicoectomy procedure itself may be successful, but the crown and/or surrounding bone may not be so healthy in a few years canal leading to the loss of a tooth that had an apicoectomy. Dental implant may or may not be the best idea. Sometimes the decision is purely a financial because you can dump lot of money into a tooth that will subsequently be extracted. I extracted 7 root canal teeth just yesterday. Some were because of failed root canals, while some were due to a badly decayed crown on a root canal tooth that had very little structure to be saved.
Typically this additional fourth canal is called “MB2.” When this canal is not filled, it is best to try to redo the root canal to find this canal that conventional and nonsurgical way. Sometimes patients have posts inside of their teeth and it makes removal of the crown very risky so the only option is apicoectomy. Keep in mind that an apicoectomy in the upper right molar as you described is also going to be near your maxillary sinus.
A very skilled endodontist will be able to guide you properly. Good luck with the move.
Respectfully,
Ramsey Amin DDS
Many years I had root canal in two pre molars. The dentist at that time used titanium rods to fill the canal. It seems that I always felt a little pressure above the roots but mostly just when I touched the area. A few years ago I was told the rods had to be removed and I was sent to a specialist who redid the two root canals. Though I have had no pain with these two teeth something did not feel right. I have had root canal before and know there is no feeling in the tooth. However, when I tap on one of the teeth it felt like I had a piece of concrete in my mouth.
Then I developed this lump on my gum next to the inside of the cheek.the dentistSaid my eye tooth, the tooth directly in front of this tooth, had an abscess and he did root canal. It didn’t and was redone. I had a ct scan done. The lump is hard and my dentist feels the tests show a foreign object in the middle of the lump. I am now scheduled for a apicoectomy with bone graft from a cadaver. I thought he was just going to remove the lump. But doing the procedure on my root, is this necessary. Do you have any idea what the lump is. Will this procedure take care of all problems. It is like I have a tooth ache in between the first two teeth and I feel some pressure. I asked to have the eye tooth pulled but was told it would not fix the lump. I have total confidence in my dentist to do the procedure but would like your thoughts and opinion. Thank you
Hello Diane,
It sounds like the lump you have the some type of pathology that requires a biopsy. Without seeing you or your 3-D scan x-rays, there is no way for me to tell you if you’re doing the right thing or not. It sounds like you or in the care of a very good dentist that you have confidence in. That is really important.
Root canal teeth that still hurt over time are generally either fractured internally or if there are additional root canal nerve endings that were not filled or could not be reached to be filled.
Good luck with everything.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Many years I had root canal in two pre molars. The dentist at that time used titanium rods to fill the canal. It seems that I always felt a little pressure above the roots but mostly just when I touched the area. A few years ago I was told the rods had to be removed and I was sent to a specialist who redid the two root canals. Though I have had no pain with these two teeth something did not feel right. I have had root canal before and know there is no feeling in the tooth. However, when I tap on one of the teeth it felt like I had a piece of concrete in my mouth.
Then I developed this lump on my gum next to the inside of the cheek.the dentist
My 27 year old daughter just had her #13 tooth extracted. She had pain and her dentist took an xray and suggested she get an apicoectomy. We made an appointment for the same day with a maxil-facial surgeon who upon examining her xray said the prognosis was poor for an apico because the infection was above the root and he said there wasn’t that much tooth left to support the post and that it likely would fail. We then opted to pull the tooth. I asked when she would be able to have an implant done and he said it’s best to wait 4 months before doing the implant because new bone would grow and the implant would be most successful as a result. Do you agree that it would be best to wait or go to someone else? My daughter’s dentist called to see how everything went and sounded surprised that she had the tooth extracted. Now in retrospect we’re thinking maybe we were too hasty in extracting the tooth. Too late now but I want to make sure that we do the right thing as far as implants are concerned. She made an appointment with her dentist for this Thursday so we’ll see what he has to say. Is there anything she should be asking him or/and do you have any suggestions? I’d like to hear what you have to say about all this.. Thank you very much.
Hello Stu,
I’m sure the surgeon had an excellent reason to extract the tooth. The tooth probably had a very poor prognosis to have an apicoectomy.
Keep in mind that doing apicoectomy requires drilling a hole through the bone to access the root and then cut off the end of the root. This removes away bone that would be used for a dental implant. Some apicoectomy is her far more riskier than others.
Just because the surgeon did not place a same-day immediate dental implant does not mean that here she did something wrong. It sounds like you saw a prudent individual that very carefully calculated your risk versus benefit ratio of an apicoectomy versus extraction and dental implant.
Your dentist is probably not well-versed in the exact procedure of an apicoectomy so just because they send to you to somebody to have it done, doesn’t mean that it can be done.
I say this in all due respect. I hope your daughter has a great experience and having a dental implant to replace her missing tooth. Going slow and steady may be the most predictable route even though it is going to take 8-12 months.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hello Dr. Amin,
In 2010 I had a fall that resulted in a broken front tooth and several of the upper and lower teeth were loosened. The broken tooth had a root canal, a crown.
[ Unrelated – In 2011 the other front tooth began to die so it also had a root canal done. This resulted in a discolouration over time despite several attempts to have it whitened. Eventually in 2012 keep them visually aesthetic, the older crown was removed and both front teeth were given matching crowns.]
This year I developed a pus boil above the original broken tooth, an xray revealed a dark area.
Antibiotics were prescribed since I had no pain in my teeth / gums – but it didn’t help. The dentist suggested to re-do the root canal but was unable to drill through the crown because the original filling was too hard. Eventually an Apicoectomy was performed. Now a month later the gum has healed but the pus boil has returned. I have no pain in my teeth or gums and the boil is easily drained but keeps returning.
I went back to the dentist and the new x-ray shows nothing wrong.
The dentist now wants to do a root canal to the tooth on the other side of the broken one as he suspects that might also be infected.
I’m just a little fed up and don’t want any more root canals on my front teeth 🙁
Is there any hope for me at all! Will this end badly if I just leave the boil there and do nothing.
Hi Candy,
Sorry to hear about your misfortunes. A tragic fall can cause a lifetime of dental problems.
You must treat the roots with the apicoectomies. Do not leave the alone. The pus is acidic and will destroy your bone. You must get this chronic dental infection under control to avoid losing the teeth and eventual dental implants. It will only get worse.
I would do what your dentist recommend.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Years ago I had a porcelain pin put into my left front eye tooth. It fell out 2x, so the dentist made sure that it would not come out again and so to say glued it in permanently. I know have an abcess form at the toot of that tooth and the dentist can’t get the pin out. What are my options?
Hello Rose,
It sounds like you have a post cemented inside of a tooth that is preventing the endodontist from doing a re-treat root canal through the crown. This is a difficult situation.
Sometimes the post can be vibrated out with what is called a piezo. If the post cannot be removed, an apicoectomy may be required or you may possibly lose the tooth.
Good Luck!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi Doctor,
Six years back I had root canal treatment on the teeth No 8 . After 5 year I got pain on that teeth. Since I am in a different country , the new doctor does not have the history of my issue. So after the X-ray he decided to redo the root canal. Even after the root canal I had the pain. So he went for the Apicoectomy. There was no pain for an year. Just from last week , I am getting the pain. After the X-Ray ,doctor said there is no crack in the root. He does not know why I am seeing this pain. He suggested me to take the antibiotics for 2 weeks. If this is not working he said we can try redoing the apicoectomy. If again this is not working , then he wanted to go with teeth extraction and impact. Since the issue is on the front teeth , I am very much worried. Are we on the right direction? Can you please help me here?
Thanks,
Raju
hi Raju,
Most vertical crack lines in teeth cannot be seen on x-ray. Even under high resolution 3-D cone beam imaging, many tooth cracks cannot be seen. You likely have a fracture which would necessitate tooth extraction.
Sorry for the bad news!! Don’t shoot the messenger!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi doctor,
I had a root canal done when I was seven years old after an injury on my upper front left tooth. In August 2013 it was infected and I had the root canal redone as well as a apicoectomy. Since then I have started Invisalign to get my teeth straight and everything was going fine until I went to get a regular teeth cleaning done and now my mouth feels as though I have the same pain right above my injured tooth that I had before I had the root canal and apicoectomy done. I am worried that this will mess up my Invisalign if I need another apicoectomy and root canal. I have an appointment at my dentist Monday, but I’m really dissapointed that this is happening. What do you recommend i do?
Thanks
Hello Jordan,
During orthodontics teeth often become loose! Teeth that have had root canals and apicoectomies often become even more loose. The teeth are supposed to come loose so that they move and then should retighten after tooth movement has ended.
This doesn’t mean you’re going to lose your teeth and have dental implants!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hello Dr. Amin,
I read your article and seem to be experiencing the problems you have written about.
I broke off a small piece of my #15 molar, which I believe already had a cavity in it and may have already been going bad, around april of 2013. I went it in to see the dentist june 31st of 2013 and had found the tooth was in fact going bad. She thought that if I had came in when I actually fractured the tooth I would’ve only been dealing with a crown. Since it wasn’t too far gone, she believed I would be able to save the tooth. And the fun begins!
So, I went to have a root canal done Aug 12th. After the RCT, I developed chronic sinusitis and the tooth was, and still is percussion, sensitive, especially in one spot of that tooth. It is the only tooth percussion sensitive. When I went back to the dentist, she said everything looked great and the RCT looked phenomenal, according the X-rays, and that the endo even found the fourth root; but, I still had the sinusitis, according to my primary, and was percussive sensitive. The sinusitis failed 3 rounds of antibiotics, starting from the first round before the RCT. The endodontist redid the RCT on Oct 16 2013. This time he filled the tooth with an antibiotic and said if that doesn’t work then he would do an apicoectomy. It’s been a week since and I still have all the same symptoms, which leads me to believe that I may need an apicoectomy.
It seems to me that my situation aligns with what your article is written about and that this apicoectomy may not work. My question is, if I go through with an apico and it doesn’t work, what is the time frame for the infection to spread to the bone to the point where an implant will act as you described? I ask this question because I am not sure how long it takes for an infection from tooth to spread to the bone.
Also, will the hole that the endo puts through the bone to reach the roots be a chronic source of problems in the future?
Is the failure rate of 40% of apicecomies based on your own data or is that statistic found in some literature I can read up on? I found this but it seemed to be of a small sample: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2502352/
Hopefully my story can help others make an informed decisions and I will keep this blog updated. And thank you Doctor Amin for writing this article. Wish you were in Tampa, FL incase I need that implant. I definitely like the fact that you have the 3-d scanner, less radiation is always a great thing!
Hi Chris,
Is sounds like your #15 is fractured or has more than 4 main canals. Apicoectomies have a higher success when performed by an expert AND the diagnosis is correct. The reality is that not every apicoectomy is created equal and very few are done in an expert fashion. Your tooth and bone anatomy is a huge factor in the success of the procedure also. There are 100’s of studies to show success rates higher and lower than 40%. You have to be careful what you read and who is writing it.
Your time frame to go to an implant depends on your unique situation. Bone infections don’t usually happen quickly. Make sure you see your endodontist every year after having the apico. 3D’s work great for apicoectomies too!
I commend your efforts…you are a smart guy!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi Chris…I know this is an OLD post, however, Im in Florida and desperate to find a skilled endo and/or implant dr as Im in a similar situation you posted here. I believe the current endo who is treating me is good and overall co concerned about my well being verse money, however, I definitely need a second opinion as he seems rather young in area of experience/expertise for my case. I have researched out board certified endo and implant demtists but very stressed regarding my next step…and in meantime im on my 7th round antibiotics and 2 completed/failed root canals-and in pain from standing ongoing absess infection at roots (at least 2/4) plenty of bone loss😕 Did you locate anyone in Florida you trusted? Any information would be greatly appreciated- thank you
Hi Dr. Ramsey,
I would like to ask you a question and your opinion. I’ve had a second front tooth, on the right upper part of my jaw done a root canal about 4 years ago, after a while a cyst appeared in the top of the root of this tooth, over the gum. The infection is still there ,so now, I’m debating to have the tooth extracted and the infection removed and be treated with boned graft, in order to be prepared for an implant or have an apicoectomy procedure be done,after hearing all the cons and future complications and not good results of it. What would you suggest for me to do ? I would appreciate your response briefly. Thank you.
Hi Dario,
The question to save or to extract is unique to your situation. I would have to see you to make this determination.
Ask your dentist which is more predictable? Which will last longer?
Consult with both a dental implant and root canal specialist.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
http://www.burbankdentalimplants.com
Dr. Amin,
I broke both front teeth in an accident 50 years ago, root canals in both and crowned in the 60’s.
They became loose and had significant bone loss, so based on my two Drs recommendations, #8 & #9 were extracted, and had socket bone grafts four months ago. The bone grafts healed nicely with no complications.
About 10 days ago I had implants placed at #8 & #9. Tooth #7 is sensitive. I called my Dr at the 7 day mark about it and he asked me to call him in another week if the tooth was still sensitive. The implant was placed a little close to the tooth according to him. My primary question is: if the tooth needs endo treatment, will it compromise the implant? The tooth has no decay and is not crowned. Or should the implant be removed?
Your insight would be very helpful in determining what avenues to pursue, thank you!
Hi JC,
Give it time. Only a 3D x-ray will help determine root proximities. Regular x-rays aren’t good enough. How is it now?
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I really wish I saw that 40% failure rate before I did mine! Mine, didn’t even last 6 month!!! Implant, here I come sadly 🙁 Another few $$ grand.. why not!
Dr. Amin,
I am trying to find a dentist and medical doctor who can help me determine the best course of action to eliminate systemic infection, namely small intestine bacterial overgrowth (SIBO), caused by toxic infection of root canals in 14 teeth. The root canals were performed 1986-1989 and have unknowingly created a myriad of health issues in the decades since. After years of seeking help from cardiologists, rheumatologists, chiropractors, gastroenterologists, dieticians, etc., I realize the source of the bacteria causing so many varied symptoms is coming from my mouth. My teeth and gums are literally buzzing (tinnitus symptom) with what feels like radioactivity. The sides of my tongue feel it too since it rests beside so much crown metal exposed from receding gums.
My dentist will not even conduct a routine cleaning without my taking an antibiotic prior to the office visit. Infection at the roots of 14 teeth is apparent on x-rays. When I approached her on the subject of the SIBO and failed root canal connection, she sent me to receive ozone autohemotherapy, with the advice that the teeth be saved at any cost.
You may guess the autohemotherapy did not work, as it is a blood transfusion, for which the blood cannot reach the dead area of the teeth. If we were to re-clean the roots of all these teeth, could the bacteria possibly all be eradicated within the miles of dentin tubules? Is there any possibility of overcoming the monstrous beast this bacteria has become within my body without removing the teeth?
I feel I am down to two unsavory choices. Live with the toxic pathogens and the disease they wreak on my body or extract so many teeth that will certainly alter the quality of my life. At least the latter would BE a life; presently I am sliding down a slippery slope of losing hope for a disease-free one. Keeping the teeth “at any cost” is seemingly the cost of my life.
What to do when so many teeth are involved?
Thank you for any insight you may offer.
Jill
Hi Jill,
Wow, what a situation you have. I would suggest seeing and infectious disease specialist in a hospital that has an associated dental school on campus. Having multiple specialists of all types working together should help you get healthy again.
Keep me posted!
Respectfully,
Dr. Amin
thank you for clarifying my question. I have decided to come see you. I talked to Angie and I have an appointment in about 3 weeks.
I look forward to meeting you!
Tara
Dr. Amin, first thank you for your posts. I can see how you help so many people. I had an apico 7/12/13 – it is now 8/22/13 and i have pain on the tooth (sort of like a bruised tooth). The scar tissue on my gums is such that it hurts to smile and laugh. Now, i have numbness sensation on my upper lip and nose. I feel pressure from my nose to the tooth (#8) My surgeon says it could be the ligament holding the tooth that is inflammed and to give it another week. I’ve been on antibiotics around the clock since 7/5/13. My concern is, if i have the tooth removed and start the implant procedure, what i can i do or ask for in order to make sure the implant is done correctly? There is a hole on my jaw above #8 from the apico – is that filled with cadaver bone or is bone from my jaw/chin best? Again, thank you for your interest in helping us.
Hi Brenda,
Wow, it sounds like you have had quite the ordeal with this bad tooth. 🙁
Your questions are really difficult to answer but….you asked about how do you make sure the implant is done correctly.
My best advice is to see a very skilled implant dentist that is has the training, experience and judgment to handle a case as complex as yours. They will help you make decisions on what type of bone to use, etc. Ideally the same person should do your bone grafting and make the final tooth. Do your due diligence…you are replacing a body part.
Front teeth are far more difficult than back teeth.
I hope you get well and get off antibiotics!!!
Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hello Dr. Amin,
I had a root canal in November 2012 on my second upper molar from the back. It was complicated, requiring an endodontist, who said I had an extra canal and that all the canals were curved. I believe he also said that I had a minor fracture. I have had some minor sensation in the tooth ever since, and recently it began to hurt while chewing hard foods and also with hot foods. I am concerned about this for two reasons. One, I;m not sure what all of my options are (try another root canal, or do an apicoectomy). Two, I don’t want to pay for another root canal, since the last one wasn’t even a year ago and it completely cleaned me out (financially speaking). If I go to the same endodontist, is it accepted professional practice that they redo the root canal free of charge?
Thanks,
Kate
Hi Kate,
If the tooth has an internal fracture it has a poor prognosis. I work with many excellent endodontists who excel at what they do.
Unfortunately if a fracture is present, even the best dentist can’t save it. You should ask the endodontist if it is worth going back inside or do they think you should extract it and have a dental implant.
Good luck,
Dr. Amin.
Hello Doctor
im 32 years old and about 7 to 8 years ago i had a apicoectomy done on my front top right tooth (second from the middle). this past week i started to feel swelling from the back (inside of my mouth) and a feeling of throbbing, and when pressed i can feel the flesh moving back and forth at the area where the cut was made for the surgery. there is no pain, it just feels numb and a little bit of swelling. i was researching and came to your site. could you please advise me what to do and what might be the problem i have, because i getting the feeling it has formed a new cyst and a new apicoectomy will be needed to save my tooth. please get back to me ASAP i dont want my problem to get worse.. thank you very much and have a great day.
Hi Armen,
Sorry to hear about your tooth. You need to be examined by a dentist to really know what is going on. X-rays are needed.
You might have a failing apicoectomy and re-infection of the area. You may or may not be able to retreat the area.
Good luck to you.
Dr. Amin
Hi doctor(respect)
one of my front main incisors have been root canaled which lasted for 7-8 years then infection recame last year
then apicoectomy done infection again recame
iam with the infection for one year
what can I do for it a very foul smell comes from my mouth
I just hate it
can you give some temporary suggestion for removing for this bad smell
Hi Sonu,
It sounds like the teeth need to be extracted. Despite the root canals and apicoectomies, if the teeth remain infected they have little hope. I would explore removing and replacing them with dental implants.
Expect to have missing bone in the area from the apicoectomy.
Good luck,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dr. Amin,
I had tooth 14 root canaled back in 2000. It did not work the first time and within weeks, it became infected and my dentist at the time retreated it. One day, this past Novemeber, I woke up with the gum above that tooth a little swollen and painful to even touch or brush my tooth brush over it. There wasn’t a pimple or pus, just swollen and the tooth was throbbing me all day. I went to my dentist and he recommened I see an oral surgeon to possibly get it extracted. He felt that if I tried to retreat it, that there isn’t the best possibility that all the infection will ever really be gone.
Well, I made the appt. with the oral surgeon, but chickened out and canceled. Shortly thereafter, everytime I ate anything sweet, that tooth would throb all day. It was even making all my other teeth hurt. So, I decided to see that oral surgeon afterall. My appt was March 4, 2013. I was starting to get nervous about the extraction and decided to just talk about my options. He told me it was a bad tooth that had an abcess and apicoectomy doesn’t always work. I reluctently had it pulled that day and I now think he just didn’t want to bother with anything else, other than me getting that implant we discussed earlier(more $ for him)
I am now in so much pain after a month and am seriously regretting my decision. I don’t even want to get the implant by him, so saw another implant specialist who says I now need a bone graft and I should get the implant soon. Do you think this was a good choice and I’ll feel beter after the implant? tmj, pain, gum problems have started since this tooth was pulled 🙁
Sorry for this long comment. I hope to hear from you.
Hi Michelle,
Sorry to hear about your dental woes. Unfortunately many root canal teeth end up getting extracted. I have even had to do this on family members 🙁
The dental implant is likely to be a predictable, long-term replacement. Please discuss pain management before the procedure. Most of my patients have a 0-2 out of 10 on a pain scale after dental implants and extractions with me.
Here is a link from a few years ago that might help you.
https://www.burbankdentalimplants.com/dental-implant-or-root-canal-cost-and-value-comparison/
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dr. Amin,
Thank you so much for your response. I really appreciate the time you took to do so. The link you recommened for me to take a look at did not show up on your reply. Would you kindly be able to post it for me? Thanks again.
Michelle
I had an apic done about 2 weeks ago. Today was the first day I actually got a peak at the area. Back upper left. The gum area above the tooth is white. It doesn’t appear swollen, just whit in color instead of pink. Is this normal? I am not currently having any pain or discomfort.
Hi Kate,
A white surface is normal healing in the mouth if it is an “open” wound allowed to fill in. White pus is not normal.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dear Dr. Amin,
I had an apicoectomy on tooth 24 nearly 4 years ago after a failed root canal.
1) It was suggested that I have the tooth splinted to the 3 adjacent teeth for support. Do you know the success rate of splinting teeth after apicoectomy?
2) Would failure of the splint mean loss of the tooth?
3) The tooth is beginning to feel more peculiar than usual. If I need an implant and there is not enough bone, could a block graft be performed?
4) I was told that if an implant is necessary, my oral surgeon commonly removes 2 or 3 teeth adjacent to the one in question for additional support. Why not place a single implant? The idea of removing 4 teeth is upsetting.
Thank you in advance for your response.
Hi Carol,
Splinting the teeth means connecting them with bridgework or resin.
If it is bridgework, I would avoid that due to connecting a weak tooth to the others. The resin splint is just meant to reduce mobility.
It sounds like the tooth is pretty bad. A BLOCK graft is very specific and is difficult to do in the lower front single tooth site due to space restrictions between roots. Removing adjacent teeth just to be able to do the graft is a bit odd, UNLESS those teeth need to go too. Then it is a good idea.
You should have a really experienced implant dentist who does both surgery and makes the tooth look at you. Front teeth are super complex and the stakes are high.
I hope this helps.
Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry.
Hi Chris,
I broke my front 2 teeth(#8,#9) when i was 9 years old. I had a root canal and crowns done then and i never had any problems until Aug 2009 which was 18 years later.
I had to replace the crowns and they found some infection (though i did not have any pain or discomfort)the doctor suggested a Re-RCT on both #8 and #9. And after 6-8 months of re-RCT when i had a checkup the doctor said #8 is not showing any recovery and we will do a apicoectomy. Though i requested him to check on #9 he said he wouldn’t touch it as its showing signs of recovery.
In Dec 2010 after he said all is well, i had the permanent crowns done. Within few months of permanent crowns i saw the gum of #9 swollen and some pus draining out. Now he said i will have to remove the tooth as it might be fractured and he isn’t sure. As i didn’t want to loose my teeth and just want to make sure with a second opinion.
In Aug 2011 another doctor said he would like to do an apicoectomy before suggesting anything else. So it was done on #9 and he said the infection is pretty nasty and hopefully it doesn’t reappear and sometimes it takes a couple of apicoectomy. In Dec 2011 i saw the pus drainage again. He saw my x-ray and said nothing to worry i continue to keep the area clean and rinse with warm saline water. Which i have continued to do so and also brush and floss twice daily.
Towards end of 2012 i started seeing the gap between the tooth # 8 and #9 becoming very prominent with each passing month. #9 has started leaning/moving inwards.
I have consulted 2 oral surgeons recently.
1. One says a better solution will be to extract both tooth, graft, wait for 4-6 months and go ahead with an implant. Meanwhile will fix me with a flipper. Gives me no surety that implant will succeed or last for how long.
2. Another says apicoectomy, but no guarantee of success or if the gap will increase or decrease.
I don’t want the infection to affect the nearby good teeth and further complicate things. I know you will have to see me in person for any suggestions. But i live in Jersey City,NJ. I do have x-rays for my tooth and would appreciate your opinion in this matter. If you are willing to check, I will very happy to email it to an id you can provide me.
Looking forward to your response.
Hi Mithila,
Based on what you say it sounds like both teeth should be extracted. If the teeth are moving and you have had apicioectomies in the past, retreating it is not likely to work.
For midline symmetry, it may be best to replace both teeth.
I would suggest you get into the hands if a dental implant expert. Preferable to have a single dentist do your whole procedure. Do your research. Front teeth are especially difficult to have long term outcomes that are perfect.
Experience is key.
Good luck!
Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry.
Thanks for your response. I had both my teeth removed in Feb 2013. However i had inflammation over #9 after the removal, surgery and bone graft. The x-rays and further small incisions in the area weren’t fruitful in determining the cause of the inflammation. After 4 such successive incisions (every 2 months to allow drainage if any), in Dec 2013 i saw some relief. And have not been seeing any inflammation since.
Currently the doctor doesn’t assure me that an implant will be a success. However he says i’m ready and implants will be the next step.
I would like your advise on such cases if an implant will be a success and the long term of the implants. If possible also please give me a reference to any well versed implant surgeon in or near Jersey City, NJ area.
Thanks.
Hello Mithila,
Go to the website http://www.ABOI.org and look for a dentist with similar credentials to mine in your area. Besides credentials, make sure that you and your Dr. get along well. You are likely to get to know each other very well!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Thank you for the link. May i ask if you seen such cases as mine and if yes or no can you say what do you think is my prospects?
without seen you, it would be impossible to know this
hi doc. i got operated for apicoectomy last week. but before 6years i have done my root canal due to cavity, so now it was infected. n done with apicoectomy. now my dentist is suggesting me for root canal. n when i asked for implant ,then he replied me ” we should first save ur original tooth. i have done this treatment to my lower grind tooth. third to visdom teeth. what do u suggest? implant or re root canal?
Hi Axay,
It is really impossible for me to tell you what to do without seeing you. Only save the tooth if it is predictable to do so. If it is hopeless, then extract it.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dear Dr Amin,
My dentist referred me to an endodontist to have my upper incisor root canal redone, where I went on 6th November. And went back 6weeks after that to finish the root canal but, I still had symptoms he redone the dressing in the tooth again. I was back this week to finish the root canal finally. Luckily had no symptoms since the dresssing was done at the 2nd time, howevere when the x-ray was taken he said the infection was still there and it will need more time to show up on the x-ray if the root canal worked or not. I remember him saying in November the infection should resolve and should improvement be seen in 3months time. Now it has been 3months since I went to him and the the x-ray was the same that he took 3months ago. I am very scared to lose my tooth!! 🙁 I am only 26yrs old! I need to go back for another x-ray in 6months. I was considering to have an apicoectomy in very near the future if the infection will still not be improving. But after having read your topic I might be better to have an implant as with apicoectomy will have some bone loss which I already have due to the infection. I just would like some advice or opinon please.?
Also my other question would be that I went ahead with teeth whitening in the past 3weeks, before my root canal was finsihed while I only had temporary fillling placed in my tooth. The specialist said it is absolutely fine to do it. Do you think so? Is it not going to slow down the process of healing the tooth? Maybe I should have waited with the whitening or it is not an issue at all.?
Thank you for your answer in advance!
Sue
Hi Sue,
The whitening of your teeth is fine.
I would probably give your natural tooth more time before jumping into extracting it or an apicoectomy. A dental implant is a close second to your god given teeth.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Thank you for having this web site and answering questions. I had apicoectomy done today and only now I found out the name and more information about it.
How is the necessity for apico determined? I had sensitivity to cold, some dull pain, moderate gum inflammation.The root canal was redone and the symptoms returned in a lesser form.The endodontist even debated that it could be the crown itself causing the problem. Could the procedure be done unnecessarily?
Hi Tina,
Apicoectomies are commonly redone. The rationale and decision to treat your tooth in this manner is made on a case by case basis.
Factors include: root length, presence of a post, pocket depth, gingival bio type, medical history and many others.
I’m sure you are in good hands. 😉
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Thanks so much for the article and please help me with a question:
I have had 2 root canals on tooth#14. It is abcessed again and endodentist recommended today to have the apicoectomy with bone grafting as there is a hole the size of a marble. My question now is…. Why does it continue to get re-infected and should I just have it extracted? From what I read in your article and some others, there does not seem to be a very high success rate and I have already spent over $4000 trying to save it not to mention another $3000 for the apicoectomy
I had a retreatment of rct#7 now I think it cracked it has crown. Shouls I pull it as soon as possible and also I have bone lost on the tooth vould I still get implant?#6 has impalnt also. By the way the endo thinks it has cracked and I’m getting pimple on my gum.
Hi Charma,
It sounds like the tooth has no hope now that it has cracked.
If #6 is an implant already you may be able to not place an implant and rather cantilever a tooth off of it.
It can be a great alternative to having a second implant and may even look better!!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, CA
Dear Dr,
I had a front tooth root canal/crown after an injury when I was 12 years old. I remember that dentist saying I would develop an infection every 10 years or so which would require cutting open my gums and scraping out the infection.
I am now 29 and a routine dental checkup revealed what the dentist called a periodontal abscess. The dentist prescribed antibiotics and referred me to a Periodontist. The Periodontist recommended removing my tooth and inserting a dental implant. Is this really my only option? What happened to cutting open the gum and scraping out the infection? The periodonist said he doesnt recommend it because the infection could come back. I’m terrified. It’s my front tooth. What if something goes wrong? What could go wrong? I’ve read a few things on the internet about possibly drilling into a sinus cavity? This tooth never bothered me until I took antibiotics. Now I feel a constant kind of fuzzy feeling above my tooth and in my right nostril. Should I get a second opinion?
I appreciate your professional opinion.
Also.. What type of dentist should I be seeing? The only specialist I went to was the referred Periodontist. Consultations run about $150-$300 for no insurance, so I want to make sure Im going to the right place. Should I be talking to a Periodontist, Endodontist, Oral Surgeon?
Thanks again!
Hi Vee,
There are only so many times you can re-apicoectomy the same tooth. It sounds like you now have bone loss in the area and the implant is probably your best bet. If it is predictable to keep the tooth, then do so. An endodontist can help you make that decision if you think you can keep it.
As for who to see, I am a firm believe that you will have a much better result by someone who does BOTH the surgery and makes the prosthetic tooth.
This is especially true in the front of the mouth or complex implants. You will also save money.
A periodontist or an oral surgeon does not do both. Find an implant dentist with at least 10 years of experience who has done a lot of implants like yours.
Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hello Doctor, I have a dilemma. I had first root canal treatment 20+ years ago. I developed an abscess and had to retreat my two upper front teeth two years ago. I have developed a huge but not painful abscess again 3 weeks ago. It was finally lanced and drained last week. I was told I needed an apicoectomy. But after educating myself on internet I am lost. I have already invested so much money on these teeth, and now I am not sure what to do. Would it be better to just pull the tooth out and put an implant instead and crown on the adjacent tooth? I asked my doctor, and she thought I was crazy :o) She said its always better to try to save your own tooth, and why would I want to pull my tooth out, I can lose so much bone afterward… But then again nobody can guarantee apico will work, and it seems like I am going to lose bone with this kind of treatment anyways, right? Would an artificial bone materials help with this if if I needed to put an implant later? And what to do in case of gum recession after apico? The treatment will involve more time, money etc… That’s why I can not make up my mind, which way is better? apico or extraction :o) What kind of incision would you recommend to avoid gum recession on front upper teeth? So many questions! Thank you
I suggest you have a second opinion. It really comes down to predictability over the long term. If saving the teeth is sound, predictable treatment then by all means save them. If you are only going to end up extracting them in three years then don’t waste your money. See a really good restorative dentist and an endodontist.
Keep in mind that having a dental implant in a previous apicoectomy site is more difficult than in an area that didn’t have one. Seek out someone really good for this!
Good luck!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Had a root canal on #7 almost 4 weeks ago by a dentist. Symptoms after root canal: tooth hurt when tapped or pushed on, also throbbed when walking/running. Saw endodontist after 2 1/2 weeks who prescribed steroids and antibiotics. Took all meds but symptoms unchanged. Endo says tooth looks good on x-ray and wants to see how tooth is doing in 2 more weeks. I think my tooth is fractured because I had intense pain during root canal when dental assistant placed a subtance in my tooth near end of procedure which was to lighten my tooth. It felt like she pushed the substance right up into the tooth and it was very painful. I told the endodontist this but she says she doesn’t think my tooth is fractured because she sees no pimple on my gum. She also says my tooth would be hurting all the time if it was fractured. She may do another root canal. If indeed my tooth is fractured, I don’t want to have a pointless procedure. What would you do if you were me?
Hi Cheryl,
Sorry to hear about your experience. If I were you, I would wait it out a bit and have your dentist continue to try to diagnose the area which may take time.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, CA
Hello Dr. Amin,
A recently had a dentist’s visit and he said my tooth#19 had cavities some time ago and was left untreated. Now it was spread a lot more and recommends I do a root canal. I am currently not in any sort of pain, and he says this is early on and we can try and save the tooth; he recommeneds a location which has less than 2% failure rates with Root Canals and he has been working with them for over 20 years (these are endodontists)
I have had previous root canals done to my tooths #5 and #12 about 7 years and ago and both of them failed in the last 2 years one after the other. I had them extracted and put in implants. One implant is complete while I am still on the healing process for the crown on the other one.
I am not sure if I need to try and save my current tooth #19 molar – do a root canal and then crown and then have the risk of having that fail too, hence I am debating whether to have it extracted and implanted like the others. Given the nature of the tooth (being molar) and having multiple roots; the RC procedure is going to more complicated than tooth with a single root. The dentist said the infection is not too bad and we can save the tooth now; but I never understand the concept of “saving a tooth” esp after RC when the tooth is dead and having a crown put on it. Why would it not be wise for me to rather have it extracted and implanted?
Given the location of the tooth and the complications with bone loss during extraction or with RC procdure and considering my dental past of 2 RC failures, what would you suggest be the better route for this situtation? Extract and implant or RC, crown and having the risk (if at all) of the RC failing? (appt in next 3 days)
Thanks a lot!
Hi Jay,
Sorry I couldnt get back to you within your time frame. Without seeing your mouth and x-rays I couldnt guide you on exactly what to do.
In my own mouth, if the tooth or teeth were predictably savable with root canals, that is what I would do. Dental implants are great, but if your own tooth is healthy enough to save, that is the best.
Make sure you get the crown and root canal done by a high level dentist. Trying to get it done cheaply will only cost you more later.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I need to make a quick decision. The right side of my face has been swollen for about 4-5 days…now finally subsiding after cross-treating antibiotics. It’s been recommended I get an apio on #4… because the post in my root canal is too big to drill without cracking the tooth/crown (the tooth was originally a cracked tooth from chewing ice). The dentist mentioned there is movement in the crown/loose tooth and he thought he saw a crack in the xray, but the endo said he doesn’t remember noticing any movement and he said he did not see a crack? Within the month, I slipped and fell down and my teeth were very sensitive that day (felt weird when sipping soda) and the following week my left jaw a couple times became numb, tingly, and painful. I saw an ortho who thought it was possible from a scan that I had a slight fracture in my jaw, but the oral surgeon follow up on a 360 showed no fracture, but a problem with #4. No pain or cyst showed up until a couple weeks later and the swelling didn’t show up until the dentist tried to see with a pick if he could help and then sanded my tooth some to prevent it from hitting the bottom tooth to help the pain. I read about bacteria leaking from teeth of root canals and the potential for health issues, but I don’t welcome the idea of another tooth being pulled either…especially because an implant would be much more expensive, and then couldn’t that get infected too or harbor bacteria? I don’t know what to do…now I read about bone loss from your site, and that wasn’t even an issue I knew about…I certainly don’t want to lose any bone. I’ve been told the first root canal was not done properly, but I think based on the sequence that the tooth or post may have become loosened when my teeth banged when I slipped and fell and then bacteria entered and became infected or whatever was happening there already got jolted and turned into an infection? I’m also wondering if I get the apio…—if the tooth/crown is already loosened, would that immediately allow more bacteria to enter and become infected or wouldn’t it matter because it would be closed off with filler? Sorry for all the questions, but I have to make a decision in the next 2 days. Thank you for offering to help with your opinion.
Hi Tammy,
It really comes down to a question of predictablity. If the endodontist feels that the tooth has a good long-term prognosis with the apico then by all means save the tooth. You must make certain that the remaining tooth structure is sound to hold a crown also. If both of these are in your favor, it is better to keep your tooth!
If it is really questionable, then the obvious answer is to extract and place a dental implant even though the cost will be more.
Good luck and keep me posted!
Ramsey A. Amin, D.D.S., D.A.B.O.I.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Burbank, California
Hello Dr. Amin,
If an apicoectomy can possibly fail, will an extraction and implant be more practical (i.e. less expensive in the long run; faster healing process)?
What possible dental problems will occur if two front teeth are extracted?
I will appreciate a quick reply. Thanks.
Hi Maria,
Your situation is a tough one to say without seeing you and your x-rays. Either way there may be some degree of compromise. Both options will have their own unique risks, benefits and alternatives.
Work with a great dentist in your area to guide you on making this decision.
Ramsey A. Amin, D.D.S., D.A.B.O.I.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi Dr. Amin,
I went in for a root canal (on #23) that was not able to be completed due to calcification near the root of the tooth. There has been some bone loss but the tooth is still stable and shows no signs of deep pockets around the gum line. I have been told that the next step would be to do an Apicoectomy with a bone graft (osteo graf) in the attempt to try to save the tooth but that there is no way to tell whether it can be performed/completed until the gums are pulled back (from eye tooth, to eye tooth).
I’m not really questioning the Apicoectomy at this point after reading up on what it is for, but about the fact that the need for the gums from the eye tooth, to the other eye tooth needs to be pulled back — For one tooth, does that much truly need to be removed, in order to get to the root of the #23 tooth?
Thank you for having this site and being willing to help all of us who are having to make such difficult decisions on what to do!
Hi Jen,
Sometimes in order to access even one tooth, the incision has to be as long as six teeth. It is important that the dentist can access and see the area very well before doing anything.
That being said, there are different surgical approaches that vary by the dentist’s their training, judgment and experience.
Ramsey A. Amin, D.D.S., D.A.B.O.I.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
I failed to mention that the abscess gets bigger when I eat and drink and smaller when i dont.
i asked the surgeon why, but he said he didnt know.
Hi Orrie,
After an apicoectomy, the tooth should be doing ok “IF” it works. You may lose the tooth and end up needing an implant in the very near future. If so, some degree of bone grafting will probably be needed too.
Respecfully,
Dr. Amin
i also wanted to mention that the abscess gets larger when i eat and drink,
and decreases in size if i avoid eating and drinking.
I have a tooth that was root canalled a long time ago.
last december i had an apicoectomy on the tooth.
the infection returned, so this past july the oral surgeon performed another apicoectomy. the infection has again returned.
i want desparately to save the tooth, if possible.
may a root canal be performed after an apicoectomy?
should i have seen an endodontist, rather than an oral surgeon for the apicoectomy?
thank you.
Hi Dr,
I m in NJ.
Is there an email id i can drop you a mail at? As i would like to send you my x-rays while i explain you the state of my tooth. Please do reply to the email id provided herewith.
– Mohana M
Hi Mohana,
I would need to see you in person to do a full evaluation. X-rays alone does not give me enough information to help you properly.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
818-846-3203
Hi Caleb,
Tooth #10 area is generally easy and sucessful to rebuild. I usally do block onlay grafting or GBR (guided bone regeneration)in my practice in Burbank to get the best outcomes.
What is going on with the teeth right next to #10? Any crowns or bone loss?
Ramsey A. Amin, D.D.S., D.A.B.O.I.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi, Today I had my front #10 tooth extracted in preparation for an implant after the tooth became reinfected (it was previously root-canaled a dozen years ago).
Upon extraction today, my oral surgeon said I’ve lost a lot of bone from the infection and that the chances for implant success are now low — he still used an artificial graft material — but said he thinks I will mostly likely need a bridge.
After reading through your posts today I feel like he is not giving me full options on other means by which to build up the bone for an implant. Are there other grafting options you can suggest for me to ask him or another surgeon about?
I am a healthy 33 year-old, non-smoker, with no other dental or bone issues past or present.
Thank you
I have had two different crowns, then two root canals on a lower middle tooth. Lastly, I needed an apicoectomy done because the dentist left a piece of the drill bit in the root canal which became infected and formed a cyst. Now, a year and a half later, I have intense swelling in the gum. I have been advised to take antibiotics and go in Monday for x-rays to see what my options are. Do you have any foresight or recommendations for me?
Hi Alicia,
Without seeing you, I could not tell you exactly. Ask your dentist what they would do in their own mouth.
Ask what is the long-term prognosis of your particular teeth.
Ask if they feel implants may be better.
Good Luck,
Dr. Amin
I have a question, I’m 26 years old, I had two root canals and two crowns put on my two front teeth when i was 14 due to a fall that happened. Well, I just went to the dentist and they told me i need a root canal and a apicoectomy and a bone graph. The tooth that needs the root canal is the anterior tooth to the right on my front tooth. My question is, Should i have this done, and have implants done or should i try this and hope for the best? I’m so scared and lost as to why this has occured. I’m young and have two young children ,this is so not fair 🙁
Hi Colleen,
Sorry for the delay in my reply.
Yes, the bump behind the tooth you mention may be a failure or it may be a localized gum problem.
Get to a good dentist asap!
🙂
Dr. Amin
Hi Dr Amin:
After an accident, I had 4 root canals performed on my upper front teeth. This was 4.5 years ago. About 3 weeks ago my palate behind one of my front teeth felt sore… nothing unbearable but i was aware of tenderness. today i’ve got a bump on the palate edged up behind my tooth. could this be a failed root canal so many years later? i’m terrified i’ve let something go (even though my symptoms are very recent) and i’ll lose my tooth (oh and i’m still paying off my veneers!). thank you for any information. it will ease my mind.
Hi Emerson,
Re-doing a root canal should be carefully determined by a dentist. There is no way for me to tell you this based on your question alone. You must be examined.
I have had an crown chipped in back of my mouth on top of root canal, I need to know as far as cost efficient, should I just get an implant vs redo of an root canal and crown
Hi Diane,
Consider seeing an endodontist for an opinion asap.
It could even be another tooth!
Dont wait on this.
Respectfully,
Dr. Amin
I had an epicoectomy done to a tooth on the lower right quadrin, not the eye tooth, but the one after that located toward the back, but is not a molar back in 2002/03.
Over the past year, that tooth has been sensitive, and mildly painful. In the past year, twice I’ve had swelling on the outside of the jawline about the size of an egg,thus swelling on the face. It’s painful, I can’t chew on that side….eventually the swelling goes down. I’ve had no insurance for 2 1/2 years…..I don’t want to wait until an emergency happens……what do you think.
Sincerely,
Diane
Hi Carina,
It is possible that there is a problem. I would see your dentist asap.
Dr. Ramsey Amin
Burbank Dental Implant Dentist
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Website ~ https://www.burbankdentalimplants.com
Visit My Blog ~ http://www.dentalimplantdentistryblog.com
818-846-3203
Hello Dr Amin,
I just had an apicoectomy, about 20 days ago. I do not have any pain and the tooth feels good, but a pimple developed right after my stitches were removed, about two weeks ago. I took antibiotics for a couple of days and the pimple went away, but now is back. Its not necessarily painful, I can eat normally, but I am afraid about what this may be.
Thank you in advance.
It is very possible! Yes!
I have been told I have to have a root canal on #19. I am also experiencing pain below my jaw and into my neck could this be from the bad tooth?
Hi Henry,
What did your dentist say at your appointment on Tuesday?
Dr. Amin
I had a apicoectomy done to me about 5 wek ago because of tooth infection didn’t go away. It’s have been 5 weeks and after I stoped taking the antibiotis my upper lip began to swollen and the right side of my nose. I’m going to see the the dentist Tuesday. Is s the extraction of the tooth wiil help to get rid off the infection.
Thank you!
Hi Emily,
Don’t fret just yet. Most root canals that are well done, heal great. They need a lot of time to heal though. Lateral incisors usually heal really well with complete bone fill. Give it about a year.
It’s the molars that cause the biggest issues! It should be fine!
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Website ~ https://www.burbankdentalimplants.com
Blog ~ http://www.dentalimplantdentistryblog.com
818-846-3203 — Burbank, California
Hello, I came across this in a google search- I just had my first root canal done (it’s my right lateral incisor), and I’m only 25. I went in for my first checkup on it today, and my endodontist told me that it doesn’t seem like it’s healing well (it’s “very stable” he said, but the bone isn’t healing as much as he’d like, and I’ve also had NO pain, swelling, or infection since it was done). He told me to come back in 9 months (a year from when it was done), and if it still hasn’t healed better then I will need a bone graft… is there any other way to take care of it? A bone graft sounds pretty serious. Or is there anything I can do to make my bone “heal better?” I have no clue what to do. Thank you!
Hi Margaret,
30 years is a excellent life span for a dead tooth!
Retreating the root canal vs. a dental implant is a difficult decision sometimes.
It depends how much of your original tooth is still present to hold a new crown and how healthy the root is.
Without seeing you and an x-ray, I can’t give you an educated response.
Consider seeing an endodontist for an opinion.
I hope this helps! Let me know if you need anything else!
Respectfully,
Dr. Amin
Hello Dr. Amin: My top front tooth ‘died’ over 30 years ago. The tooth was bleached 2x and eventually I had root canal work, post and crown, all which lasted many years. Most recently the tooth became loose and fell out. One dentist said the work on the root canal did not go deep enough making the post too short and not as strong as it could have been. I am having conflicting information regarding a new root canal. One dentist said I do not need a new root canal as the tooth already had one. Would you recommend I re-do the root canal, post and crown or should I think about an implant?
Thank you for your time and consideration,
Margaret
Hi Kristina,
Generally an x-ray will be taken several months later to check the healing. The dentist will check the gums in the area also. A failed apicoectomy may not have pain so give it some time.
If you need to remove the tooth, a same day temporary bridge can be made. You will wear that for a few weeks, then the final molds can be made for the real bridge or implant crown.
Hi,
Can I please ask a question.
Ive had a Apicoectomy 10 weeks ago, i go to the cons in november to findout if it worked, but would i know now really if it worked? if i had pain?
Also if i needed to have my tooth taken out(front) how long do i need to wait till i can have a bridge?
Thank you lots
Hello I had root canal treatment on my pre molar, canine and incisor. Nevertheless I had an inflammation that involved the first 2 teeth I mentioned and had apico about 4 weeks ago. Now I feel some dull pain at times and some tingling on my jaw. Is that normal or?
give it more time to heal.
That’s really interesting. Thanks for the info.