This article is a follow-up to a video from 2009 that I receive a lot of questions about. Block bone grafting for dental implants is still a very successful procedure…. But a lot has changed over the years!
(side note: Many people mistake the term “graft” with “graph.” The correct term is “graft”)
Basics on Block Grafting
I highly suggest you watch the video and read this post. You’ll gain excellent information from both to help you make an informed decision if this is something you’re considering.
A block bone graft is done when there is a large section of bone that is missing. That area of missing bone is usually the outer wall of bone that faces your cheek. A block bone graft is needed when there is no way to put particulate bone particles into a “hole” like an extraction socket. The block bone graft attaches by screws to your jaw kind of like an orthopedic surgeon who is fixing a broken leg with screws. The screws are only kept in during the 4-6 months that the bone is reconnecting to your own existing bone.
Where you get the bone from ? Using your own bone is the best. But for smaller grafts, human tissue allograft can be used.
Advantages of Human Donor Bone Blocks
Over the last 15 years doing block bone grafts for dental implants I have used a combination of human donor block bone graft (allograft) and block grafts from your own body (autograft). Using block bone graft from your own body requires that I have to cut a piece of bone from your chin under the roots of your lower front teeth) or from the area where your lower wisdom teeth are or used to be. Cutting this piece of bone has its own risk factors especially the risk of permanent or temporary numbness because the nerves are close to the area where the bone has to be taken from. Using bone from a tissue donor has an unlimited supply so we don’t have to worry about the bone taken from these areas as not being enough.
Block Graft From Me
What experienced dental implant surgeons around the world have agreed upon is that block bone grafts using your own bone tend to be “avascular.” This means that they do not have a good blood supply…unless they are THINNED with purposeful space underneath! Getting blood into the bone graft to bring it back to life is the key to success of a bone graft. Even though the bone is taken from your own body, sometimes that outer wall we call cortex is too hard and does not get good permeation of blood vessels called capillaries.
The addition of molecular enhancers and growth factors made from your own blood has also changed…. technology is evolving!! The use of L-PRF, PRP and PDGF made from your own blood tremendously helps a block bone graft. These are made from drawing a little bit of blood at the beginning of your IV sedation and concentrating your own natural growth factors from your own blood . The growth factors and even stem cell will be reimplanted into the bone graft area…. This is truly awesome.
Bone From Another Person is Dead
Accredited tissue banks have learned how to properly harvest this bone also. The type of bone I use has origin from the vertebrae (back bone) of another human being. Remember that this bone is 100% dead. Nothing is alive in it. It has undergone severe radiation treatment to kill everything. Your own body will make it alive again. Some small gaps around the bone graft may be filled in using cow bone which is also very safe and well documented over several decades now.
What hasn’t changed is the surgical ability to do this procedure and the ability for you to heal very well. This is definitely a procedure for a very advanced dental implant surgeon with a lot of experience. This would not be the type of bone graft for novice. You as the patient must also be healthy. Smoking , substantial alcohol use and diabetes would be significant risk factors and lowers the success of any dental bone graft and implant procedure.
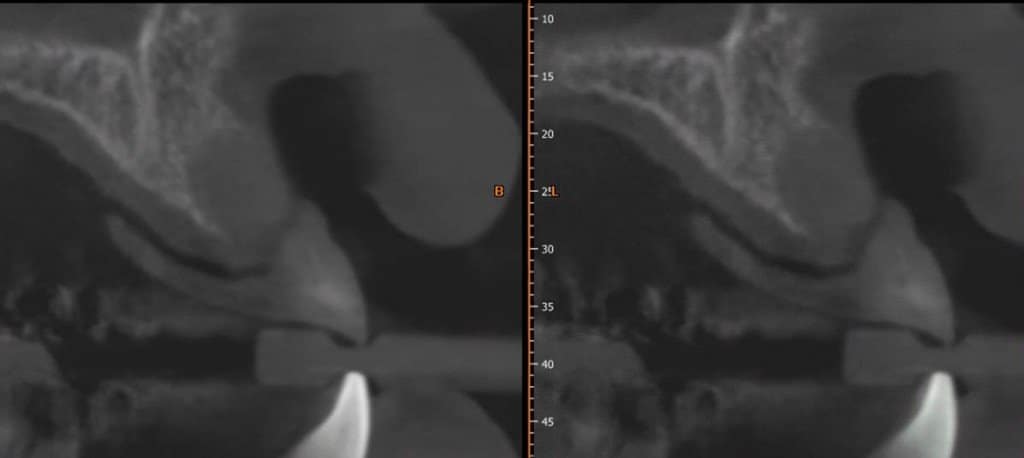
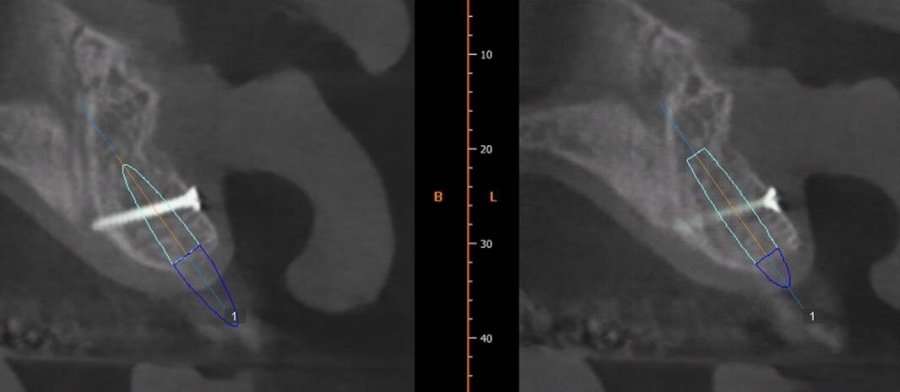
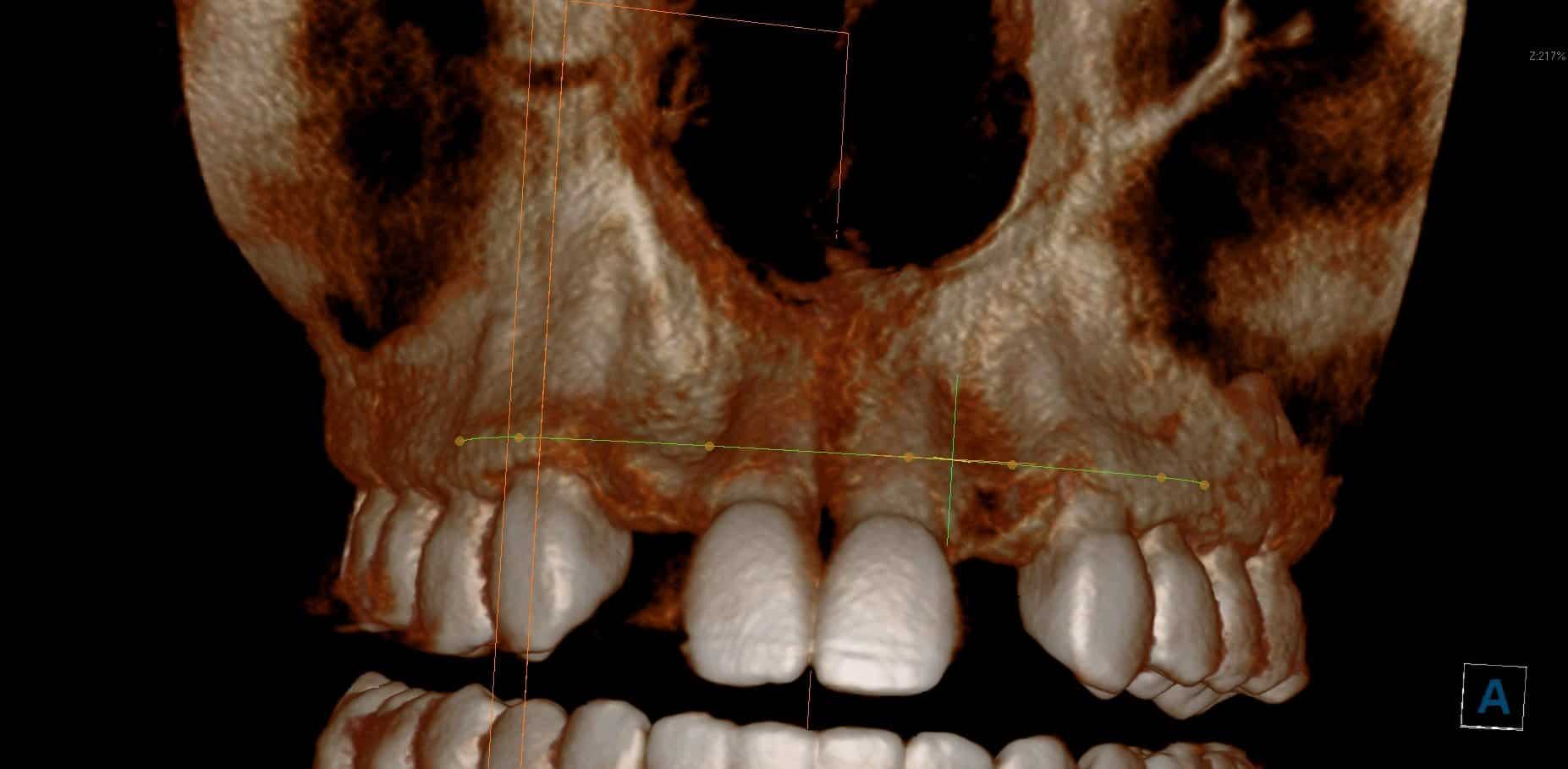
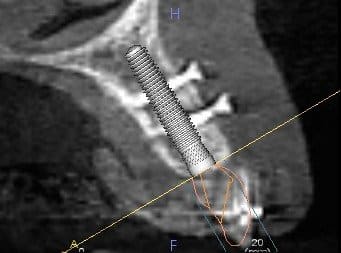
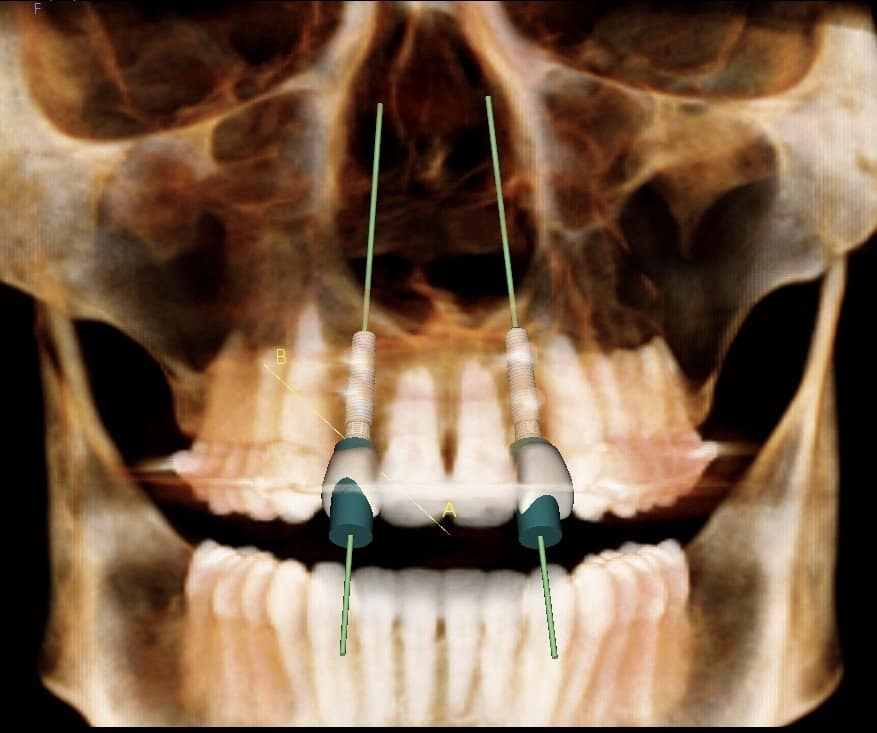
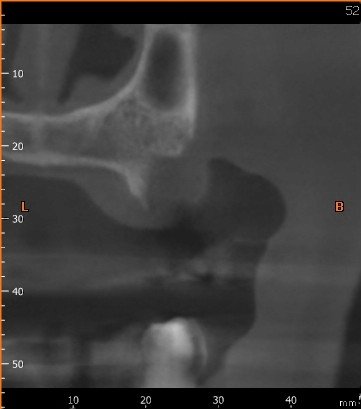
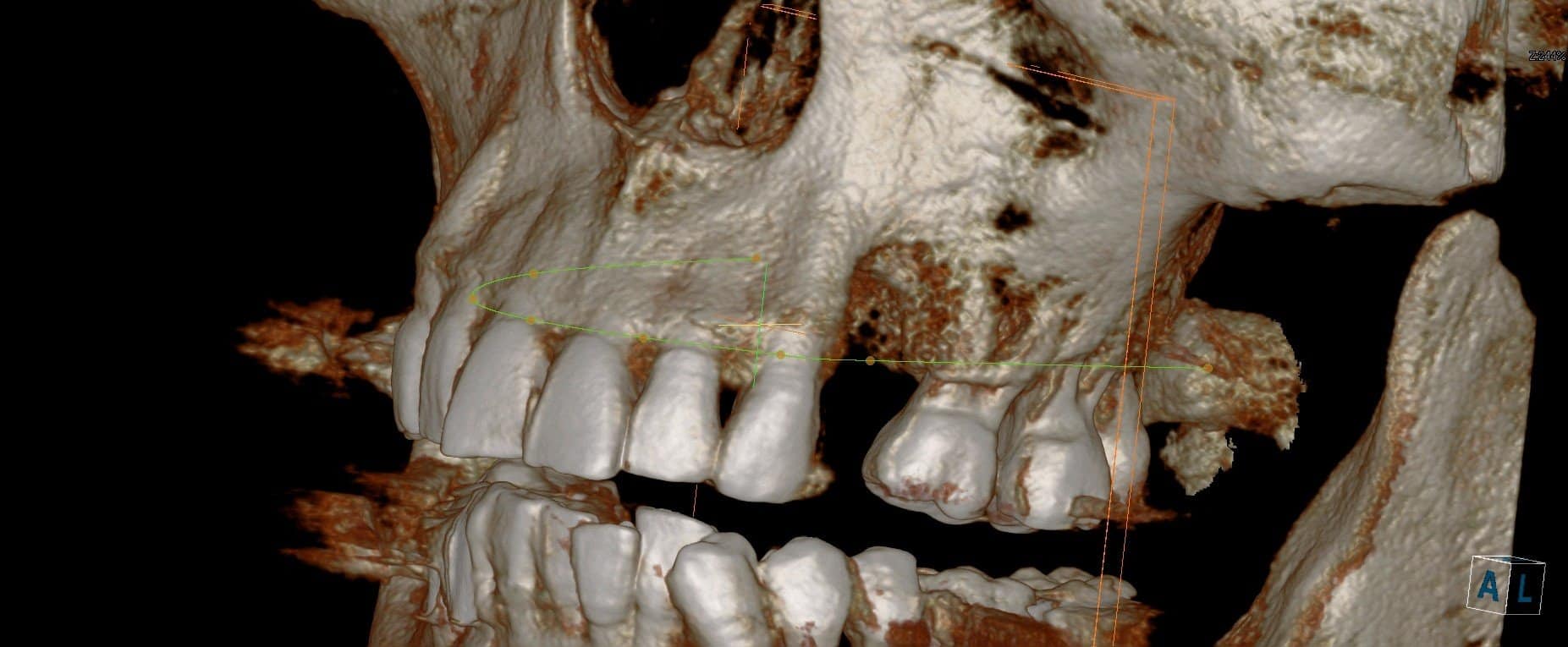
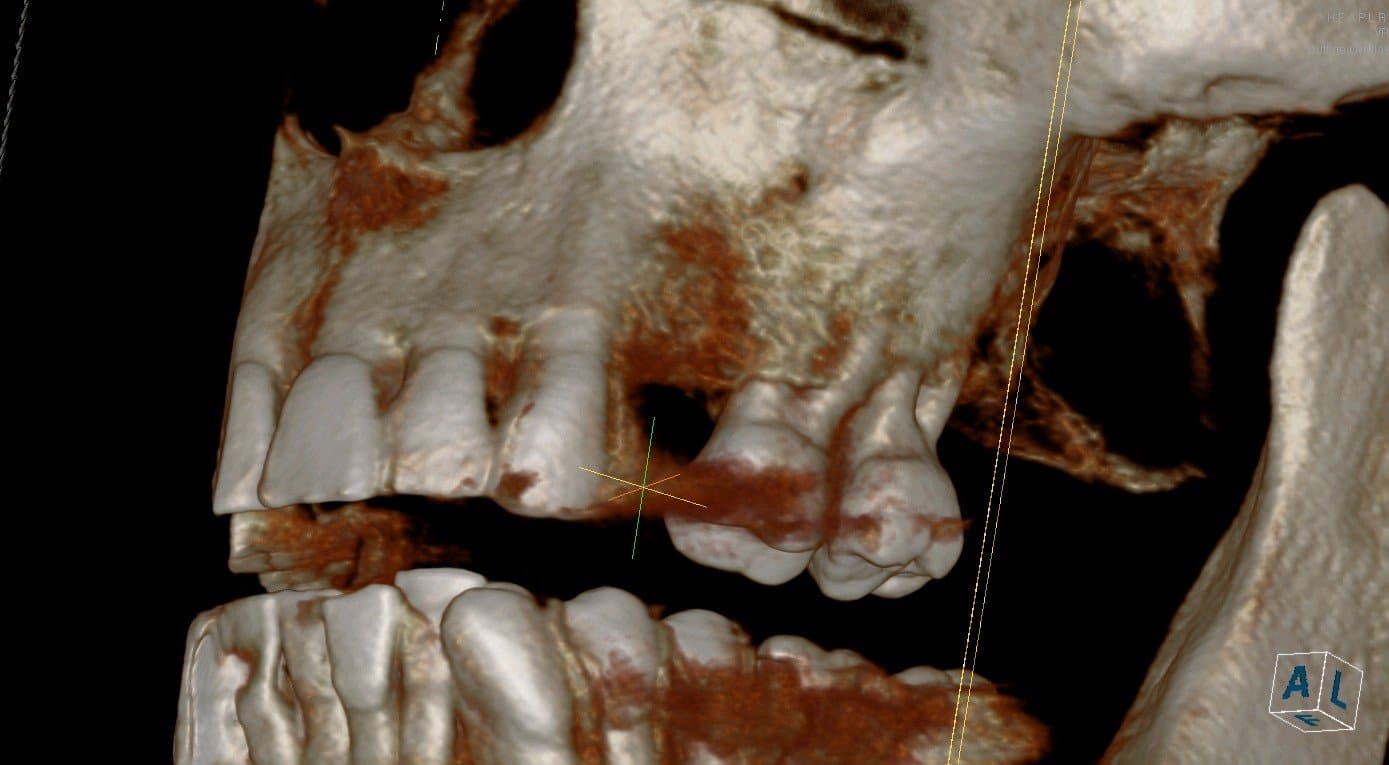
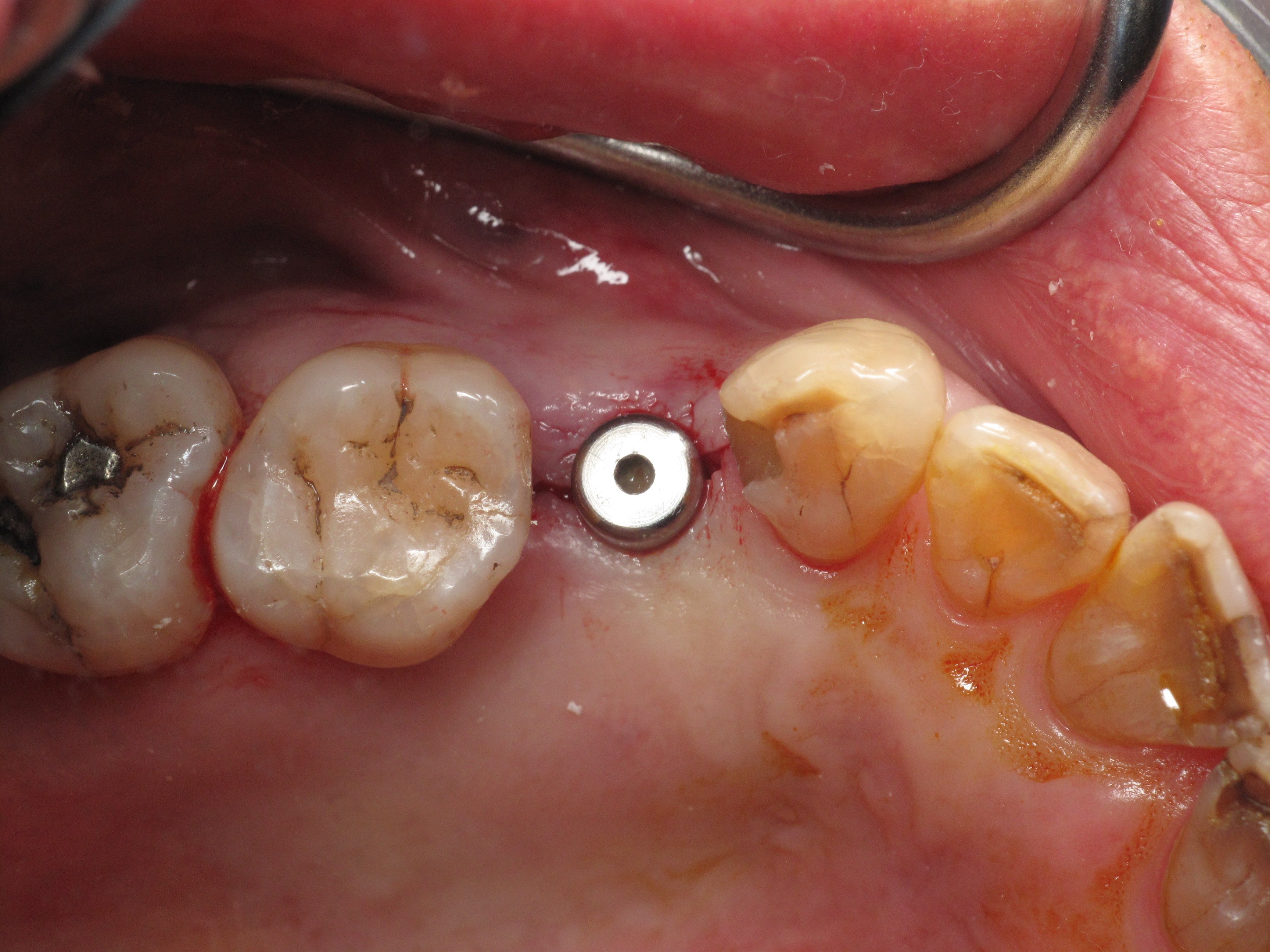
The examples shown should help for you to understand why a block bone graft is done. On the first images you can see the bone in cross section taken from a 3-D scan. The bone is too narrow to accept the diameter of the virtual dental implant which is outlined over the bone. In order for dental implant to be successful there needs to be an abundance of bone especially on the outer wall of the implant for it to be stable long-term and last a long time. You can see on the images where the bone graft was completed and the screw is holding in the bone.
Block Bone Graft Procedure
The gum is lifted, your own bone is prepared in order to receive the cadaver bone and that block bone graft is then screwed to your existing bone. The bone graft is hydrated in your own natural growth factors before it is screwed to your bone. The gum is passively covered back over the top and the block bone graft is allowed to heal for 4-6 months prior to removing the screw that holds the bone graft and placing the dental implant. A special type of temporary must be used for this bone graft if it is for a front tooth.
You can see the massive addition of volume that was added. The 3-D scan that was taken after the bone graft shows that same outline implant now sitting in a proper amount of bone. This will make the dental implant procedure extremely successful from a biological standpoint and from a cosmetic standpoint. When all of the bone is present both vertically and horizontally, there will not be open black triangles between the teeth which can be unsightly especially if it is the upper front area. The teeth on either side must have very healthy bone levels for this to occur. You cannot do a bone graft next to unhealthy teeth.
Block bone grafting using human tissue allograft from a cadaver is no longer a last ditch effort. Of course there are so many different ways to rebuild bone from bone widening expansion, socket bone grafting, sinus lifting, nerve repositioning, guided bone regeneration with membranes










…. So there is no one solution for everyone. Your case must be studied carefully to determine what is going to be the safest procedure with the best outcome.
The block bone graft for dental implants is typically done in areas of the upper front and side teeth. All photos are surgeries performed by me.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry

Hello Dr Amin
I went thru some very scary times with dentist’s so after I had many surgeries and braces I couldn’t take anymore pain ! I made the worst decision of my life pull them all ! I was 18 and now 65 I have probably severe bone loss on the bottom can you help me I would gladly book a consult if you think I have a chance
Thank you
Susan
100% you can be helped!
this will help 😉
https://burbankdentalimplants.com/dental-implants-without-bone/
Hello Dr. Amin, I have severe bone loss in my upper 4 front teeth. Teeth 7 and 8 have no bone left due to infection, are loose and need extracting. Tooth 9 has the most remaining bone and can be saved. Tooth 8 has some bone but cannot be saved. The Periodontist wants to remove all 4 front teeth, try a bone graft and implants but I could be with flipper for a year with no guarantee this will work. Im wondering if it would be best to get a bridge fron 621 with 7,8,10 Pontiacs? I don’t want to go through a year of removable appliance and the expense if there is a chance this won’t work. What are the percentage that grafting and implant dont work when there is little to no bone. Thanks
A 6-11 bridge is a great option in your situation. See this post about it!
Hello
I have severe bone loss in my lower front jaw. ( first 4 teeth) this is due to a untreated gum abscess and advanced gum disease.
Would you be able to restore this bone vertically and horizontally with a block bone graft procedure?
The other teeth surrounding are healthy and have healthy bone.
Yes. I do a lot of these complex cases!
Hello
I have severe bone loss in my lower front jaw. ( first 4 teeth) this is due to a untreated gum abscess and advanced gum disease.
Would you be able to restore this bone vertically and horizontally with a block bone graft procedure?
The other teeth surrounding are healthy and have healthy bone.
Yes. I do a lot of these complex cases!
Hi, I would like to ask about implants. I was in a accident about 15yrs ago. Since then I have lost all but 7 teeth. I have had significant bone loss over the years on both top and bottom. Since there is so much empty space in my mouth, is it possible to still get a bone graph?? Can you tell me how many graphs can be placed in a person’s mouth to have successful placement of implants? Thank you in advance for taking the time to answer this question.
This is a great question. The answer is exactly opposite of what you may think. When you have so few teeth left is actually better not to graft and often to level the bone instead. This will allow implants to be placed into a more solid location without having to go for full bone grafting, have a better result, and keep cost low. Many of these cases I do with zygomatic and pterygoid implants on the top jaw in order to make it so that you have implant bridges the same day the teeth are extracted
Dr. Amin,
I had tooth #11 removed due to fractured root, tooth had root canal/crown placed over 30yrs ago. I am 48yrs old and very healthy. I had a bone graft/immediate implant placed Feb 2020, the area had significant bone loss, including bone loss on side of #10. About 3 wks later my periodontist discovered the implant was loose and it had to be removed. He placed another bone graft, same day and just went back to have sutures removed. I am supposed to go back Mid June to have scan to check bone development. He now is thinking a bridge may better as he stated the tissue/gum will recede and due to bone loss tooth would be high in gum My smile is “mid range). My upper front teeth are healthy other than area with issue, #11,#10. I really don’t like the idea of a bridge. Is there anyway to develop vertical bone is this area? Or any option to try to get a implant? I am in the Minneapolis area and I’m not finding anyone here that appears to have the experience as you do. I am willing to travel when this virus thing passes, if needed. Thank you! Jen
Vertical augmentation is certainly more difficult then traditional horizontal bone grafting which just add width. It is certainly possible! It in fact is even more successful in the upper jaw than it is in the lower jaw. This is something that I do all the time. It is very technique sensitive and most dentists do not provide this service as they lack the experience, judgment and/or training.
That being said growing bone does not happen overnight. Vertical bone grafting often needs 7-9 months of healing and oftentimes secondary bone grafting at the time of implant placement. In addition to that, a gum graft taken from your palate is often needed because the gum has been stretched to fit over all this new bone. It is really going to depend on the health of the adjacent teeth. If the other teeth have truly 0 bone loss then chance of success is very high. This can be done via block grafting, guided bone regeneration-GBR, titanium mesh, vascularized pedicled bone flaps etc. Each case is very unique.
Stay safe during COVID 19! I would be happy to see you as a patient.
I’m kind of in a bad situation.
I had a bad infection in two upper front teeth but they were not salvageable and were removed, leaving a rather large gap between the teeth on either side. My current dentist tried a block bone graft but it
failed to attach. (Why, I don’t know, but I don’t believe it was monitored enough.) Meanwhile, I went to another DDS for a second opinion and he did not recommend another attempt at a block graft. Both dentists
are now recommending a bridge, but it turns out the would-be anchor teeth are somewhat loose from bone loss as well.
My current dentist has me scheduled for deep root cleaning and then we wait and see. I am wearing a flipper right now. I am also scheduled to extract another tooth on the side of the infection. I don’t know
if it can be replaced.
I have had implants done successfully to replace other teeth. I would like implants or something besides partials or dentures to fix my immediate problem. I am prepared to continue with deep root cleaning as necessary.
I can have very recent scans sent to you on request.
Another technique that works well would be to use a very thin sliver of your own bone rather than cadaver bone on the outside. The middle can be sandwiched in with cadaver bone but the outer portion of the block can be your own taken from the side of your jaw. Typically the cadaver bone graft work very well but they are technique sensitive meeting that the dentist has to have a lot of skill this to work well. If you smoke this is certain not to work.
Hi there,
Can a block graft be placed over a socket graft on a bottom pre-molar? For example, if socket grafting was already done immediately after extraction, but I am not satisfied with the height outcome and am looking to gain back 1mm-2mm so teeth could be more aligned at gumline, is it possible to place an appropriate-sized block graft, or something else can be done?
yes!
Hello Dr. Amin,
I lost my front tooth #8 when I was a child (20 years ago). Now that I am able- I currently undergoing dental implants. I needed a bone graft prior to implant placement. I had a block bone graft placed from my right lower jaw to my middle upper jaw. Day 4 post-up I noted my gums are still dark red, and now turning a yellow/white color. My stitches appear to still be intact, and I do not see any actual bone exposure. Is this how gums heal normally after this procedure? I am just seeing granulation tissue? I am still swollen, but not in any pain at all at the actual graft site. Still some discomfort at the harvest site.
Thanks!
Ann
what does it look like now?
Hi doctor,
I see this is mostly for upper teeth. Would block grafting ever work on a lower molar #19? Large bone loss in that tooth and currently have pink porcelain crown over implant but wanted to know if this was an option.
Yes! block bone graft can be done as well. But there are many different options such as a GBR and bone expansion widening. Every situation is different!
Thank you for the response. I would be willing to redo it if I can get it better, but I was told it’s already merged in the bone and not worth risking the present bone for a back tooth. I was told it’s extremely difficult to regain lost bone height on lower back teeth, and the lack of blood supply means trying to graft it higher is not going to sustain. Is this debatable?
Yes vertical growth is more challenging in the lower back but there are predictable, long lasting ways to do this.
Any way I can email my x-ray and see if it’s worth coming in for?
Hi doctor, I live in Modesto (central valley) and was wondering if you would be able to perform this procedure on the lower front teeth. I am 30 years old and I have lost a lot of bone in my bottom teeth to the point in which they became loose and had to have them bonded with a ridged wire. I’ve been to several dentist and they’ve told me that they don’t perform this type of surgery because its very exotic. According to them, they would have to build up the ridge (height and width) before attempting implants as they are afraid my jaw will collapse. I don’t want to end up toothless or have to wear dentures so I am looking for help.
I have done 4 of these this month already. They work great!
Hello Dr. I was wondering if you know of any doctors using this procedure in Spain, particularly in Valencia Spain. If not, what resources are available to search out a qualified surgeon who uses these latest methods.
Thank You,
Peter
I’m not certain from the international standpoint. I have colleagues all over the world I don’t know a personal reference in Spain for this exact procedure.
Is there anywhere in the Southwestern suburbs of Chicago where they use cadaver block bone? My surgeon just informed me that I need this, although he never said a word before, and wants to use my jaw and I am against this.
Thank you,
Donna
hmmmmmmmm…..
Hello. I am scheduled for a maxillary bone block graft to prepare for a five implant supported 8 unit bridge. The dentist I initially saw did 4 implants with socket grafts, all of which failed after 8 months when he was planning to uncover the implants. He said they failed as I waited too long to come in for the uncovering. I waited until his billing mgr. Was able to correct billing errors that would have made me ineligible for ins. Payment for the implants and bridge. She billed my temp. Flipper as a permanent prosthetic, ins. Paid then as an alternate procedure. She had to refund both my insurances in order for them to agree to cover the work planned. So this prolonged my treatment. The dentist extracted 2 of the failed implants and referred me to an oral surgeon for bone block graft and implants after healing and for the extractions of the remaining 2 implants. He said he will just do the bridge. Problem is that while I trust the oral surgeon I have lost trust in the dentist who referred me to him and I am afraid he will not do the bridge correctly. The first flipper had teeth so small and caved inward, I looked like I had no teeth. After insisting, he agreed to make another one.But at first he said ” I am not a fan of big teeth”This temporary flipper still does not fit right after 1 yr. And looks awful, like I have no upper teeth alough an improvement compared to the first one.. He has religned it but refuses to make a new one and keeps saying, wait till after the bone graft, that he will shave off some of the top so it does not to have the graft. He seems to only be concerned with function. I am a mouth breather, so my lips are open always and I must be conscious now to try to change that, otherwise, only my bottom teeth show. My mouth area is large, so bigger teeth have always looked great and we’re closest to my own. Previously I had a bridge but after many yrs. The abutments failed So, I have considered getting a second opinion on the graft as, while I trust the oral surgeon, when I adked about options to the graft, he said “There are none.” I feel that my care is fragmented and prefer to see a dentist who can do all the work. I did locate a DDS and want to schedule a second opinion. I am concerned that if I request my records, ( the oral surgeon and dentist seem to know each other well)that both will tell me to go elsewhere and if the second opinion dentist cannot do all the work, I will have to find another oral surgeon.Another issue with the dentist who did the failed implants is that he has no interest in my other teeth, I had to ask about a cleaning !And a few times he used an exam room with no sink or paper towels, I had to keep going into the bathroom to rinse my mouth and put the flipper back in.Am I being unreasonable to expect more and wanting to change providers at this stage of the procedure?
Yikes!!! I can see why you would want to change providers….I would too! You are not locked in.
Thank you. I needed this reassurance.
Dr, is there any hope, assistance & affordable way for me to address my severe bone resorption due to wearing full dentures since 22 – now 57 and now causing me various health issues and at risk even fracturing what is left of my lower jaw during normal day to day activities? I currently have employment and need to stay employed.
you may want to consider seeking treatment had a dental school in your area.
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
How much does it cost normally to have a block bone grafting? Can I wear dentures while healing as I need to go go work?
This depends tremendously on the size of the graft that is needed. Yes, you can wear some type of temporary but it needs to be relieved so that it absolutely 100% does not touch the graft while it is healing during the first six weeks
I had bone grafts and 2extractions and implants last week in my front upper. My lips appear much thinner and the distance between my lips and tip of nose is longer than it was. I look older and different. Is this temporary, a result of some remaining swelling, and/or might get corrected when stitches are removed? I also don’t show as much of my teeth when I smile now. I hate the way I look.
This is likely a function of how the teeth were made. Remake them more like your old teeth and the problem will go away.
Thank you for dental implants tips. We all appreciate your information. Keep posting these kind of nice blogs….
I recently had a block bone autograft from the lower left jaw to correct the defect left from extraction of 2 poorly placed implants in the palate behind the upper front ridge (#8&10). I had been told that the periodontist who originally placed the implants placed the implants prematurely in a massively resorbed alveolar ridge. A split ridge had been done with bovine powder and implants were placed at the same time, too close to the adjacent natural teeth. Unsuccessful attempts at restoration led me to the implant extraction. The implants were removed, a block graft performed and amniotic membrane and growth factors used instead of PRP and BMP (surgeon said it would minimize swelling and prevent the gum from opening.) The gums were detached from canine to canine and pulled down and over to cover implant extraction sites as well. Immediately after surgery I complained about severe tension to the upper lip, in fact, now 3 months post op, the inner top part of the lip is now the gums on upper ridge. There is still marked tension in the upper lip and bottom part of the nostrils. There is also a nagging pulsating sensation in the area where an apioectomy was performed on #7 at time of surgery. Is this normal? I also notice the membrane material showing and can feel a hard line on the gums upon soft touch with my finger. Brushing and flossing is painful. There is sometimes pain in area #6-7 teeth and bone. Surgeon says gums still remodeling, but I have concerns about the lip anatomy, the gums receding around canine #6, and constant pulsating on the surgery site #6-7. Should I insist surgeon perform gum graft to release tension and correct new recession to #6? Would a periodontist be best to correct, or is this something the oral surgeon should correct? Greatly appreciate your insight.
Hello Maria,
I’m sorry to hear about your misfortunes. It sounds like you are in good hands now. A block bone graft often requires an extensive release of some of the tissue below your lip in order for it to stay covered. I tell most of my patients is lasts about 1 month. After 2-4 weeks you should have pretty much 0 pain. Something is likely going on, but I don’t think releasing the gum at this time is the right thing to do. I would take a 3-D scan to evaluate the current healing. Keep in mind that not all apicoectomy procedures are successful. A lot depends on the original root canal being very good for the apicoectomy to be successful.
The attention near the nostrils and that whole area naturally loosens and remodels. In 15 or 16 years of doing this procedure I have never had a patient that did not have this natural soft tissue remodeling occur. The lip is oftentimes used to cover over the large bone that is placed. The implant insertion appointment, the lip tension can be relieved by repositioning the gumline back to its original location.
Good luck, I’m sure things will heal up well. I don’t think you need to change implant dentists.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dear Dr Amin
11 days ago now I had dental implants fitted in Budapest. I also needed some slight bone augmentation,
This was carried out and I was given stitches both for my implants and bone augmentation.
The implantologist told me to have stitches out between 7/10 days. As I’m home from Budapest I had to find a local dentist. To cut a long story short. When I had stitches removed the dental surgeon removed all 12 stitches between my two implants. Then informed me that my other stitches were not there. These stitches were located above my left maxillary cuspid and my left maxillary bicuspid.
Of course if they’ve just come out this is great news but as not dissolvable stitches if have snapped and some is behind gum still could this cause infection? Is it likely that they would have snapped under the gum and still be there?
Should I get this checked out?if so would doctor be ok?or would it be better to see a dentist?
It’s just I’ve already taken a lot of time off work for this and spent a lot of money so don’t want to go for check up if most likely worrying over nothing.
Thanks for your time
Jon
– See more at: https://www.burbankdentalimplants.com/block-bone-graft-for-dental-implants-2015-update-ramsey-amin-dds-reviews/#comment-42771
Yes, infection can be caused by retained stitches. A dentist should remove these rather than a doctor.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Hi, 11 days ago now I had dental implants fitted in Budapest. I also needed some slight bone augmentation. This was carries out and I was given stitches both for my implants and bone augmentation. The implantologist told me to have stitches out between 7/10 days. As I’m home from Budapest I had to find a local dentist. To cut a long story short. When I had stitches removed the dental surgeon removed all 12 stitches between my two implants. Then informed me that my other stitches were not there. These stitches were located above my left maxillary cuspid and my left maxillary bicuspid.
Of course if they’ve just come out this is great news but as not dissolvable stitches if have snapped and some is behind gum still could this cause infection? Is it likely that they would have snapped under the gum and still be there.
Should I get this checked out if so would doctor be ok or would it be better to see dentist.
It’s just I’ve already taken a lot of time off work for this and spent a lot of money so don’t want to go for check up if most likely worrying over nothing.
Thanks for your time
Jon
Yes, infection can be caused by retained stitches. A dentist should remove these rather than a doctor.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dear Dr. Amin,
What are your thoughts on a single dental implant, linking both upper central incisors?
I had my front left tooth (upper central incisor) extracted recently due to an infected root canal. There is some bone loss from the infection, and the site will be bone grafted in 6 weeks. I have been told to consider extracting my right central incisor as well due to poor long term prognosis. It had a vital pulp therapy performed 20 years ago. It is still vital, but very fragile under the crown. A prosthodontist suggested that I keep my natural tooth, and have it root canal treated. However I am leaning towards extraction, as recommended by the periodontist (for predictability). Also, I would like to avoid issues of future root canal infection which may compromise the implant next to it.
The periodontist that I consulted with brought up the idea of a single implant (in my upper left central incisor), linking to my right central incisor. This will bridge both central incisors together
Will a dental implant bridge in this scenario be any different than individual implants in both sites? Will there be aesthetic and stability issues in the long term?
I would not suggest this for UPPER central teeth. It can and should be done for some LOWER central incisors. Uppers are too big, the cantilever force is too great, and it will not look good unless it is so unique.
I’ve been missing four teeth (all the molars) on the bottom left side of my mouth for five years. At this point, I’ve had considerable bone shrinkage. I’m looking into implants and know I will need bone grafts. Also, my facial symmetry has been affected by the bone loss. My jaw is much smaller on my left side of my face and it’s beginning to look much different from my right side. Will bone grafts and eventual implants help to restore my facial structure on the left side? And, if so, which type of bone graft procedure? If bone grafts and implants won’t restore my facial structure, symmetry, and volume in its entirety, what other procedure will I need to achieve full restoration?
Hi Cai,
It sounds like you have a combination of vertical and horizontal bone loss in the lower back jaw. This is a particularly difficult area to build back especially if the bone is lost vertically. Many female patients that have been facial bone structure and thin skin may have a more collapsed appearance when teeth are lost.
Without seeing you and a 3-D scan, it would be impossible for me to tell you exactly what to do. Try having and inexpensive removable temporary partial denture called a flipper made. If this filled in the space, then having implants in the area should do the same. The design is going to have to be critical on the teeth to be able to fill in the facial voids. You may even need some pink porcelain if the teeth are tall and vertical bone cannot be rebuilt. Sometimes these areas are so bad that a nerve repositioning needs to be done.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dr. Ramsey,
Thank you for the detailed reply! I just recently had a CT scan taken, and it’s in my possession. My local dentist took a look at it and said that he believe I have enough bone to get three implants without bone grafts. However, I’m doubtful of this because my friend’s father–a periodontist–told me that I would probably need the grafts. Granted, my friend’s father didn’t see the CT scan; he just looked in my mouth. Anyhow, I’m looking for a second opinion. If I sent the CT scan to you, might you give me your opinion? If there is a fee involved, that’s fine.
Cai
Hello Cai,
Please contact my office directly at 818-846-3203…. Asked for Sophia. She can review some details for you.
Take care.
Dr. Amin
Hi, I am so happy to have come across this site. Unfortunately I am in ND otherwise I would be booking a consult. To make a long story short, I am almost 32 & was in a car accident almost 20 years ago. Lost several upper teeth, got implants at age 13, they failed over the next 10 years causing significant pain and chronic infection. I have had multiple grafts, of all sorts, my own jaw and chin, cadaver, and synthetic, all failed. I am told due to the chronic infection. I had the implants removed 3 years ago and thank god I did, I am not getting violently ill anymore. Since removing them I have had several other surgeries, the last being the debridement and removal of old grafting hardware. This left me with massive bone loss and the scary thought of it progressing over the years. I know that I need to place implants to prevent further bone loss (& I am sick of partials!) even though I am not in favor of them. I have seen numerous OMS providers and keep being told I have a very complicated situation and need a block graft, from the hip due to the amount needed, complicating this is significant scar tissue filling my upper jaw and left cheek. I have done some research on these types and honestly am not finding a lot of positive information, although you tend to hear the negative more than the positive. Any words of wisdom is greatly appreciated. Thank you for your time.
Hmm… Implants at 13??? That is unheard of!!
It is so extremely rare to have as much problems as you have had. You should have a full medical evaluation done to make sure you are 100% healthy. You need to be checked for bone turnover markers, Vit D and many other subtle things.
Usually 4-6 cadaver blocks will fix anything without going to the hip. It is very complex and you can’t wear any temp teeth for a while because your case is so major and unique.
Wow. This is an awesome post. I am a dentist that took one of your courses a few years ago. You have only gotten better Dr. Amin. I plan on seeing you at your next lecture in May 2015.
Darell P. DDS
Hello Darrell! Thank you for your very nice words. I’m looking forward to seeing you also. It has been a few years. I am flattered that you will be traveling all the way from the East Coast to see me speak at the dental implant conference in May. See you then
Ramsey Amin DDS
Dear Dr. Amin,
I have been reading your replies to many questions online and thought I could send one of my own. I’m not sure if this is the right address to send it to to get a response I’m hoping you will answer.
I had a bicon dental implant placed over 15 years ago to replace tooth #29. The buccal wall is mostly gone with thin tissue covering the threads only for at least 4mm. Bone is good on the other sides. I am having pain as my main symptom. I visit my dentist every six months and he never noticed this happening.
I don’t have many options where I live. The oral surgeon I saw said we could try a graft over it but can’t say how it will work to grow bone over metal spanning a entire face of an implant.
We can watch and wait.
Or we can begin two phase process. Remove implant (he hopes not to have to drill it out but hasn’t removed a bicon implant before)
Then do first graft with particulate bone scraped from my jaw (no platelet spinning available)
stage two is to place block implant from my jaw.
Do you have any thoughts or advice?
My fear with traveling out-of-state for care is if I get an infection or have any complications that will require another trip which could be difficult with the distance.
Sincerely,
Ruth
Hello Ruth,
The Bicon brand dental implant has very deep fins that engage the bone. It is not likely that it can be backed out by just reversing it if your bone is dense and being in the lower jaw. It may need to be cut out. I cannot say for sure you would need a bone block graft…. I would remove it and graft the area at the same time the dental implant is removed.
It may be very possible to save the existing implant as long as there is not vertical bone loss and the position of the outer wall is deeper than the adjacent bone walls. I’m sorry for sounding so technical, but this has to be looked at very carefully. This condition is call peri-implantitis. Attached is a link that will help you understand what it is.
The underlying problem with your implant is not the brand, but rather your existing bone was probably not wide enough in the first place. I go to great lengths to avoid this from ever happening although sometimes it can be impossible especially in a very compromised area. I am assuming you had a 3-D scan done for evaluation.
What is Peri-implantitis and What Do I Do About It? – Bone Loss Around Dental Implants ~Burbank Dentist, Ramsey Amin Reviews
Also tooth #29 area can be difficult for a block graft because the main nerve that give sensation to the jaw exits in this area. There is more of a risk of nerve damage in this particular tooth. You may want to seek another opinion before you remove the implant so that you can be more comfortable with your decision.
Most dental implants last for a very long time. It is unfortunate that you have gone to the situation. Sorry for your trouble
Very Respectfully,
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry
Dr. Amin,
I am thankful to find your site. I have a pocket facial cracked root on tooth 31. I first discovered it when a small bump formed near the tooth root. One surgeon recommends CT Scan, having it extracted and immediately getting the bone graft and implant. He said entire procedure takes one hour. I went for a second opinion and that surgeon recommends antibiotics 3 days before surgery then remove tooth 31 and bone graft it and stitch it up. Four months later do the implant. They explained the infection needs to be gone before doing the implant. since I have differing opinions which is the best sugestion? Both said I had very long roots and was a good candidate for the implant. Thanks!
Without seeing your current CT scan I cannot answer this question exactly. The main thing to consider when replacing tooth #31 as an immediate, same-day dental implant is that the nerve is deep enough in the jaw that it will not be affected by an implant.
Most people have a shallow nerve in this area making a same day implant is not possible. I have though replace this particular tooth and a same-day procedure but does not occur often. Tooth #31 and tooth #18 are second molars and are not as common for same-day replacement.
I would probably say go with the second surgeon because it should never be a race to replace a back tooth. Sometimes you need this type of speed for an upper front tooth but the last molar and the lower jaw should be approached with caution because of the nerve and other important anatomical structures that are right nearby.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry