Not All Extractions Need Bone Grafts.
A socket bone graft is done at the time of extraction to preserve the bone from shrinking. If the tooth is extracted and left alone, the bone will literally just melt away starting at just a few days after the tooth is removed. The keyword for a socket bone graft is “preservation.” This is called “bone atrophy.”
Pros and Cons of Socket Bone Grafting:
So how do you know if you need a socket bone graft or not? The most critical zone of the mouth where socket bone grafts are extremely important are all of the front teeth to the middle “bicuspids.”This is because the bone on the outer wall of these teeth is much thinner than it is in the molar region.
Keep in mind there is massive variation from person to person on how thick the outer wall bone is. Your genetics play a huge role here. Some people have naturally thick outer walls of bone and some people have naturally thin bone which does not do well for dental implants.
Some Have Genetically Thin Bone

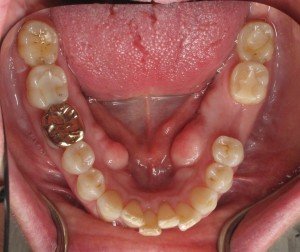
Patients that have thin bone tend to have thin gums too and are easily prone to recession around their teeth and or future dental implants. Patients that have thin bone and thin gums, have to be slightly overengineered in order to have long-term success with dental implants. Bone grafting for a person with a thin bone/gum “biotype” is always necessary. The outer wall of bone has to be designed in such a way that it is more resistant to shrinkage. This can be done by various surgical techniques and by using the right bone material for your particular situation. Not all bone is the same!
When the existing outer bone plate is thin, it is almost a guarantee that the bone is going to collapse as soon as the tooth is removed. This is because the tooth root is supporting that very thin wall of bone. So once the tooth is pulled, the bone collapses in order to close the socket. This leaves you with a depression of bone in that area. Without correction or prevention of that depression in the first place, an implant would have to be placed in a non-ideal position instead of in the center.
So what about the molars… those are the teeth that are extracted the most!! On many occasions the tooth being extracted has had a root canal. It may have abscessed and is painful. When an abscess occurs bone is often naturally dissolved the way on the outer surface. If the tooth being removed too infected, and has thicker bone, a bone graft may not be necessary or advisable at the time of extraction.
Ultimately the decision to do a socket bone graft for dental implant depends on the training, judgment, and experience of performing socket preservation bone grafting on a regular basis. Not only performing the procedure is important, but evaluating its results both on 3-D scan and how the bone feels at the time of implant insertion. And most importantly, how does this bone holdup long-term? I have personal experience of seeing the results of these procedures for the last 20 years as of 2020. The techniques that I use work well and last a long time.
Ramsey A. Amin, D.D.S.
Diplomate of the American Board of Oral Implantology /Implant Dentistry
Fellow-American Academy of Implant Dentistry


Hey Doctor; hopefully you can see this comment and help me.
I am having braces and 4 premolar extracciones must to be done.
My question is.. my ortho recommends bone graft in my extractions to preserve bone loss but my regular dentist says that it is unnecessary cause that’s the point of extractions; to create an space to move the teeth. I am a 36 years old female with all my teeth in perfect conditions but crowded in the front.
I can’t take a desicion because l can’t find someone to explain me if the risk of having bone graft is worth it; or if there are risks or long term effects.
If getting bone graft is better than not getting it.
Most of the time people extract teeth and don’t get bone graft; another thing is l don’t even know what kind of material they are putting in my mouth. I am considering stopping my orthodontist treatment because l just don’t know if really the bone graft is the best option for me.
Ortho said there’s 10% chance of losing bone dense; but there’s chance to get complications from doing the bone graft plus how is he gonna move my teeth after the bone graft if you must to leave the bone graft alone to heal(l read this somewhere) I am very confuse.. plus the difference in prices from extractions alone and extractions with bone graft is big. hopefully you can guide me a little bit… l’ll be waiting a few days until l take a desicion. I am in LA. Thank you in Advance Dr.
Honestly I would go and see a different orthodontist. Removing premolars is not done very often anymore. Removing the premolars restricts the jaw shape and can compromise many things long-term such as the size of your airway. I understand that sometimes it is absolutely necessary because of severe crowding but most contemporary orthodontist have moved away from this extraction for orthodontics.
Hi,
I had a root canal on #30 on August 28th. It failed after taking clindamycin and trying steroids. On September 19th I went to an oral surgeon who removed #30 and placed a bone graft. That morning I took 300mg of clindamycin and rinsed with Chlorhexidine mouth wash.(which I had been using twice a day for a week before the extraction)I had a very bad stomach upset and managed to get 3 doses of clindamycin 300mg in me and phone the oral surgeon.They told me to stop taking the antibiotic but did not call in a replacement which made me nervous. A few days later I had some tenderness in the tooth behind it and they called in the z pack. I had 3 days of the z pack and started vomiting. The next day I went back to my oral surgeon who proceeded to pull the gum back and look for an abscess, nothing was found and I was put back on clindamycin. I again got about a day and a half of the antibiotic. A few days later I ended up in the hospital with an ulcer. I am now doing better, but I am still having jaw pain, socket sensitivity, tenderness if pressure is applied to the gum and a small tender bump on my jaw where the extraction/graft was placed. I had a CT without contrast in the hospital which they said looked fine and I am showing no signs of infection. (no fever, gums not swollen) I am worried that almost 5 weeks out and I am still having pain and something is terrible wrong that is being missed. Could my body be rejecting the bone graft? Could I have an infection in my jaw bone that is not showing signs yet? Any suggestions would be greatly appreciated.
There is a very good chance that you are not actually allergic to penicillin. You can actually add metronidazole along with a penicillin derivative or use a newer generation cephalosporin type of antibiotic. It is likely that you have some sort of infection that cannot be seen. I would also suggest a probiotic that is yeast based to help with your stomach. Clindamycin can cause something called C. difficile. I try to avoid it whenever possible. I hope you are getting better.
Hi Dr.Ramsey I’m a 53 yrs old male that’s missing 5 of my teeth 3 of them are inthe upper back part of my jaw in which you can’t see them at all missing and the other 2 are inthe lower front part of my Jaw where you can see them clearly missing at whenever I open my mouth and talk my question is can 2 implants be placed where the 2 .missing teeth are at even though gum shinking has occurred now because I didn’t get a socket bone graft when both the teeth where extracted and now the bone has shinking to where I think I need a socket bone graft and the ridge of my gum widen so that 2 implants can be placed into my jaw bone
This is a great question Fred. It very easy to do a bone graft even though you did not have a socket graft. Keep in mind that the socket graft was intended to preserve and prevent you from getting the bone loss that you have now. A bone graft can be done to build the lost bone back and to have the implants put in.
This page on bone grafting may give you a good start for understanding the process. Please watch the video as well.
Stay safe during COVID 19!
I had a socket bone graft done after a tooth 19 extraction to prepare for a future implant. The (I’m guessing) collagen membrane fell out while I was sleeping three days post surgery and my dentist office is closed until the next day. Will it be okay for this to be open for 24 hours?
Yes. Not ideal but will be ok hopefully 😊
Tomorrow morning I will be getting my ( Third) bone graft for my upper left molar. My body apparently absorbed the cadivor bones and the post is loose and coming out of jaw because there is nothing supporting the post any longer. Is it unusual to have this procedure done 3 times !! ?? Since my body keeps absorbing the cadivor bones, is there another option ? Any information on this would be appreciated. Thank you.
To be honest it sounds like you need to see a more skilled implant dentist. This is not common
Thank you for your honest opinion. I actually thought this establishment was the best skilled in the area. Is there a website that can show where to go for the “best skilled” in an area ?
Thank you for your honest opinion. I actually thought this establishment was the best skilled in the area. Is there a website that can show where to go for the “best skilled” in an area ?
https://www.burbankdentalimplants.com/how-to-choose-an-implant-dentist/
Hi Dr. Amin,
My lower first molar was extracted this week Monday (dentist said a deep cary on the root made the tooth unsalvageable). After the procedure, which was uncomplicated, the oral surgeon said that I had good bone there and that I would be fine for an implant in three months or so. He did not irrigate or scape the socket, left it as is, and did not mention anything about socket grafting, which was not done.
Now I’m wondering if I should have asked to have some bone material put into the sockets post-extraction.
Is it still possible to do socket grafting two weeks after the extraction?
I am going to call the oral surgeon’s office on Monday but it would be great to have an opinion from you also if possible.
I also wonder what the benefit in terms of % more bone versus natural healing would be, and what the risks of the procedure are and whether it’s worth going through the discomfort and being reset back to zero day healing again (as I imagine he would have to scrape the sockets before grafting?).
I’m a 45 year old healthy male, in good shape generally though dentally I have suffered substantial gum recession and bone loss in the front teeth, stabilized the past few years with regular deep cleanings.
Thanks for this great content.
Jim
YES –but just give it time if it is a molar. A bone graft can also be done at the time of implant placement.
Hello,
When lower tooth was extracted it was bone grafted and GTR and the gums along with the extraction area and adjacent tooth seemed to have risen and started reforming something to my pleasure. A week later it’s back to where it was before extraction. Does this mean anything?
Possibly. Too early to tell
Just want to write thanks so much for answering all of these questions from everywhere!!!
You are a god send!
Hello, I read your blog and impressed with information. I have question regarding my implant procedure going on. My extraction and bone grafting have been done in past Nov2015, now I have to go for implant but my doctor is saying that I am losing some bone but not giving proper explanation for that. Is that ok if I go through implant even though I am losing bone ? Need your advise on this.
need more detail on what “loosing bone” means. If you’re just losing surface graft particles that is a completely different story than losing the main part of the bone graft which would support the implant both functionally and cosmetically.
Hello Dr Ramsey Amin,
I had an old short post that fractured the root under a crown so opted for an implant on ul5 which was small tooth so had to have the smallest thickness implant to ensure there was room between adjacent teeth to keep the papilla healthy. I am very happy with the appearance of the crown on the implant. My implant was placed over a year ago, 12 weeks after extraction apparently there was plenty of bone and my implant was placed.
It has been very stable since and looks a great fit on the gum line – there are no black triangles. but I do wonder why there is a slight dint in the gum if I run my fingers over my gum, in comparison to feeling the roots of my adjacent teeth on the other parts of the gum, which pads the gum line out, when I had a socket preservation? I wondered is this normal – or is a socket preservation not meant to preserve where the roots stuck out as such if you have thin gums anyway? All my roots do literally stick out of my gums as I have thin gums. So you can see them and feel them very obviously.
My dentist put in the powdered bone and a collagen plug and stitches after extraction. Apparently my extraction went seamlessly and the blood stopped quickly etc. I was asked to go back in after a few days and then weekly for monitoring for 8 weeks and everything was fine and three months later my implant went in.
However on reflection I remember the collagen plug coming out after a day or two (which the dentist knew about as he spotted it). Now I wondered is that dent left in my gum/restructuring of the gum normal with an implant especially for someone who has thin gums with roots that are bulky through them? Or is this because that collagen plug came out, so could have been avoided?
I have images of my mould so you can see the impression after the implant had been in a few months and where it looks sunken. Also a couple of pics of my gums with a normal picture taken today – I would like to post these however I cant seem to find a way to post them here?
I would hugely appreciate your advice. Just to put my mind at rest either way :@)
Thank you
Yes. I saw your images. It looks like you had a well done procedure overall.
You did lose a tiny bit of bone due to your thin bone gum bio type. The collagen plug likely had nothing to do with it. The type of bone that was used can prevent this in most cases.
In thin bone situations, adding more cow bone to the human cadaver bone helps prevent collapse of the bone. It is too late for that, but fortunately you have a near perfect result.
The root prominence can still be added if you wish. This is usually done with a gum graft. The graft can be cadaver or taken from your palate. It can then be slipped into the deficient area to bulk it up a bit. That tiny bit of bulk makes a big difference in a front tooth.
You don’t have to do anything also. It is your choice.
Good luck. Thanks for posting on my blog.
😉
Dr. Amin.
Thanks so much for responding and taking the time to look at my images. I really appreciate it :@)
It’s put my mind at rest as I was worried if it was going to compromise the long term success of the implant having the slight depression from the other teeth by not having the root sticking out.
It was a putty that was used so I may have got that wrong about it being cow bone but it’s good to know there is an option of gum graft should I ever need it. Sometimes I think when I’m talking it creates like an air bubble /squelch effect maybe against the action of my cheek talking against the depression, which can be distracting at times. However I may get used to this.
I may post again somewhere else as I have an interesting and large apicoectomy procedure done 20 years ago in my teens after a sporting accident and I’m unsure whether to implant it now or wait to see how long it holds out. I’ve never had problems with it but I was told they don’t last for ever.
Thanks so much for your help. You’re the best! :@)
Hi I have pus on pre molar which is a baby tooth and doctor has told me that he has to extract the tooth and do the implant later. There is a small pimple on my gum and pus is keep cmg from last one month.
I am scared please suggest what I should do?
Remove it. You will do great!! 😁